Most insurances do NOT require a prior-authorization. However, upon booking a session with us, our support team will verify your benefits to determine if a prior authorization is required.
Prior authorization is required for Tricare Primary Active Duty Members (IP is the military personnel)
If you have Tricare Prime Active Duty and the active duty personnel is the IP (identified patient) then a prior authorization is required when seeking counseling from a civilian provider such as Overcomers Counseling. However, family members of the Active Duty member do not need prior authorization.
Visit our cost page to learn more about our fees and accepted insurance here.
Insurances we accept:
We also accept EAP (Employer Assisted Program) and victim's compensation.
Insurances that we do NOT accept:
A copay, or copayment, is a fixed amount that you, as the client, are required to pay for each counseling when we bill your insurance. The exact amount varies based on your specific health insurance plan.
A counseling session will usually have the same copay as a PCP (Primary Care Physician) visit and/or an Office Visit. If you have a copay plan, you'll sometimes see your copay listed on your insurance card.

Absolutely!
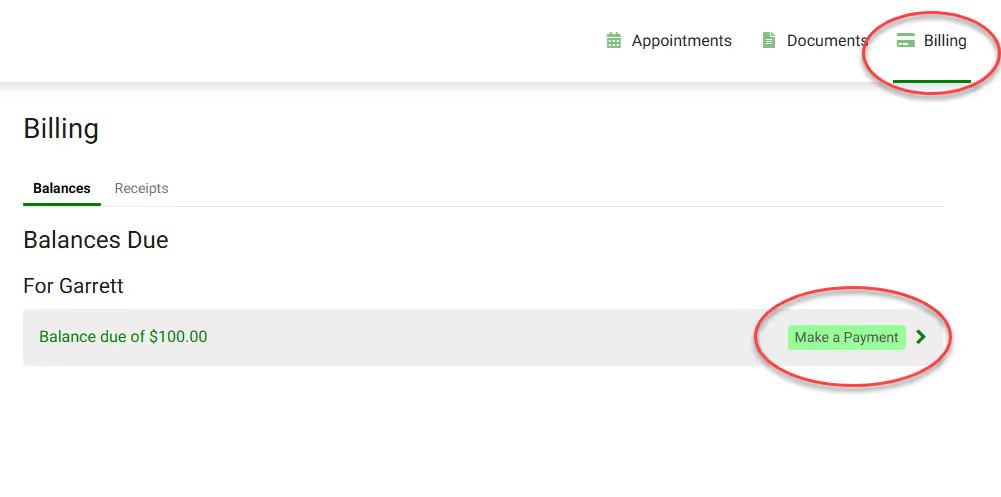
We understand the session fees, insurance cost can be challenging to understand. If you have qustions our Billing team will happliy address any issues. The best method to contact them is via the Client Portal.
You may also call or text our main line at (719) 345-2424.
Clients can pay for their sessions via credit card, debit card, or HSA/FSA cards in the Client Portal.
You may also put a CC on file for automatic payment at the time of your session! Complete the Payment Authorization form to store a card on file!
