If you have called your insurance and the representative told you that your particular counselor is out-of-network, that is because we submit claims under our group name (Overcomers Counseling) and/or our clinical admin (Jennifer Luttman, LPC) and both of which are in-network. We accept most major insurances and will provide you an estimated cost prior to your session.
Your deductible will vary depending on your insurance plan. If you have a copay plan, your deductible does not need to be met. If you have a coinsurance plan, typically, your deductible will need to be met before insurance will share in the cost for therapy.
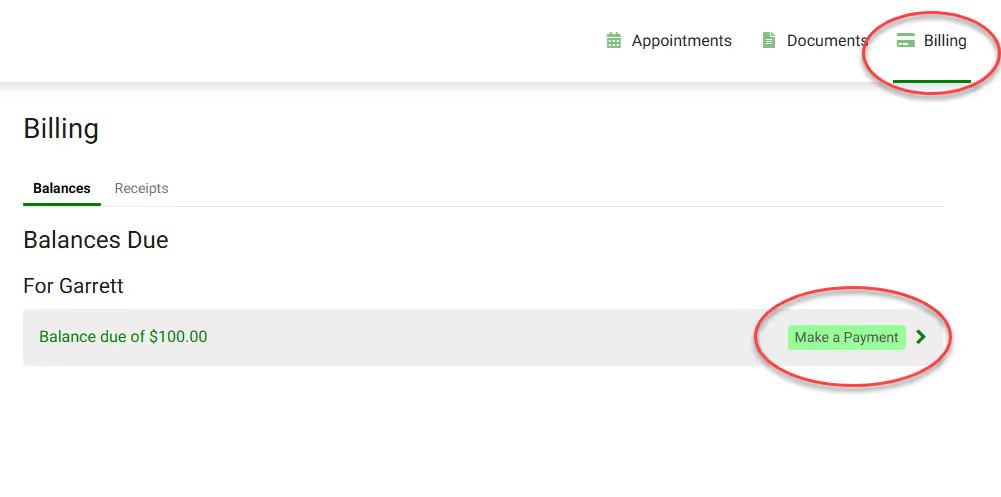
Clients can pay for their sessions via credit card, debit card, or HSA/FSA cards in the Client Portal.
You may also put a CC on file for automatic payment at the time of your session! Complete the Payment Authorization form to store a card on file!

In most cases, a referral from your PCP is not required unless you are a Tricare Prime Active Duty Member.
Yes! Family therapy is covered through Medicaid.