Depressed people often complain about problems with concentration and memory.But how does clinical depression affect the brain? And how can it lead to...

Depressed people often complain about problems with concentration and memory.
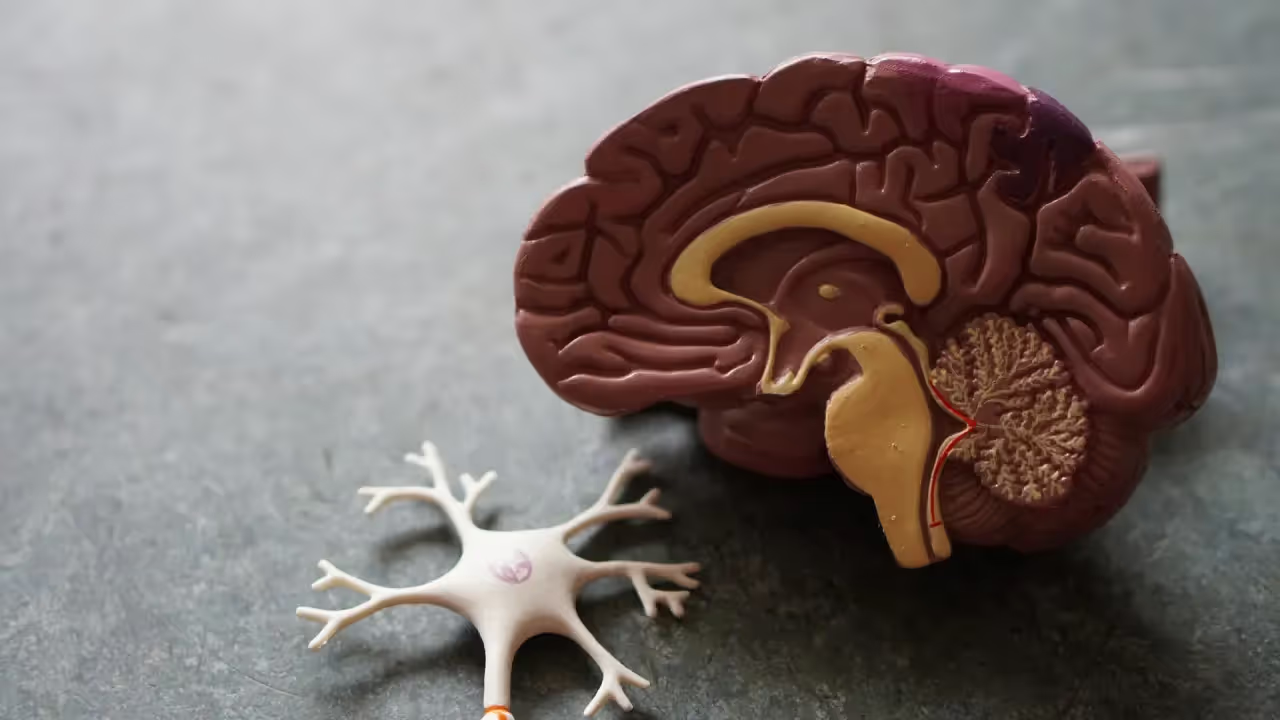
But how does clinical depression affect the brain? And how can it lead to cognitive deficits?
Depression involves changes in certain chemicals in your brain called neurotransmitters.
Neurotransmitters send messages between brain cells and affect your moods and emotions.
If you're depressed, your brain may not be able to make enough of the neurotransmitters serotonin, dopamine, and norepinephrine, or it can't use them effectively because of another problem with your brain chemistry.
Insufficient levels of these neurotransmitters result in clinical depression, whereas increased levels of these neurotransmitters are associated with improvement in depression.
Worried about if your depression could be damaging your brain or the possible effects on your brain function?
This article outlines the ways clinical depression affects the brain so you have a better understanding of this mental illness.
Clinical depression, or major depressive disorder, is a type of mental health disorder that can cause many different symptoms related to mood, physical processes, and thinking patterns.
These symptoms usually persist for more than two weeks.
In most cases, they last for months or even years.
Some people experience only one episode of clinical depression during their lifetime while others have multiple episodes over time.
Clinical depression is a serious condition that can be difficult to treat with conventional methods alone.
However, when combined with an integrative treatment plan, it can be much easier to treat this disorder successfully.
You may feel sad, hopeless, worthless, or tearful during this time. Y
our sleep and appetite may change and you'll have little to no interest in activities you normally enjoy.
While it's not entirely clear what causes depression, many factors can contribute to developing the condition.
Sometimes it starts with just one event – like a loss of a loved one – but other times it can be caused by multiple events occurring over time, such as multiple losses or traumas, or certain personality traits like being overly sensitive or self-critical.
It's important to note that clinical depression is not caused by someone being weak-willed or lazy; it is caused by chemical imbalances in the brain that develop over time from genetic predispositions and environmental factors.
The symptoms of clinical depression can include:
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), clinical depression exists when five or more of the following symptoms are present for two weeks or more:
If you have been experiencing five or more symptoms for two weeks, it may be time to get help from a licensed counselor.
The sooner you ask for help, the faster the healing process can begin for you.

A chronic mental disorder, clinical depression affects the way you feel, act and think.
Not only does it impact your mood and sense of self-worth, but it alters your cognitive abilities as well.
Let's look at some of how this condition can harm the brain, as well as what you can do to help heal it.
The Brain Shrinks
Another way that clinical depression affects your brain is by causing it to shrink in size.
This is especially true for people who have had repeated depressive episodes over a long period.
As a result of clinical depression, the brain can begin to shrink in size.
Specifically, a study published by the Journal of Psychiatry and Neuroscience revealed that participants with major depressive disorder had smaller hippocampi when compared to those who were not depressed.
To perform this study, researchers took MRIs from both groups and made their observations based on these images.
For reference, the hippocampus is responsible for processing memories and regulating emotions.
Studies have shown that its shape can change over time due to stress exposure.
Many people with clinical depression experience brain shrinkage.
This includes the hippocampus, which regulates learning and memory.
The amygdala also shrinks, which regulates emotions. The prefrontal cortex also shrinks, which controls decision-making.
Depression can lead to a reduction in gray matter volume throughout many parts of your brain, including areas associated with motivation, memory, and cognition.
This can cause a variety of issues related to mood regulation, memory retrieval, problem-solving and other aspects related to self-control and executive function.
It may also be linked with an increase in stress hormone receptors in certain regions of your brain.
Brain Inflammation
Your brain is essentially built up of a network of nerves that communicate with each other through chemical messengers called neurotransmitters.
When you have clinical depression, the cells in your brain lose their ability to regulate these chemical messengers as efficiently as they should, leading to feelings of sadness or being blue.
Depression has been linked to inflammation in the brain, which may be partly responsible for impairing decision-making skills and executive functions.
People with clinical depression have an increase in inflammatory markers in the brain compared to healthy individuals.
This causes the body to release chemicals that irritate the nervous system and cause widespread inflammation throughout the body. This causes changes in brain structure which affects mood and behavior.
When inflammation occurs, this could also cause irritability, fatigue, difficulty focusing or remembering things, or other mood issues and physical pain.
The longer these symptoms persist without treatment, the more likely they are to affect other parts of your life and relationships with others.
Finding ways to reduce inflammation in the brain may be an effective treatment for depression.
Clinical trials are underway to test this theory, using anti-inflammatory drugs or lifestyle interventions that might also decrease symptoms of depression.
One of the most common chemical changes in the brains of depressed people is a decrease in oxygen levels in the prefrontal cortex.
This area of your brain is responsible for higher-level thinking skills like planning and decision making.
It also plays a key role in social behavior and personality expression.
A lack of oxygen to this part of your brain can explain some of the key symptoms of clinical depression, including reduced ability to concentrate or make decisions, and loss of interest in pleasurable activities.
This is because of low levels of norepinephrine, a neurotransmitter that helps cells use oxygen for metabolism.
It also helps us fight our flight responses when we hear loud noises or experience other stressors.
People with low levels of norepinephrine often have trouble sleeping and concentrating on tasks like reading or watching television.
They might also struggle with fatigue and general malaise (feeling unwell).
Neurotransmitters are chemicals that pass messages between nerve cells or neurons.
These neurotransmitters carry signals between the brain and the rest of the nervous system.
In addition to affecting memory and emotions, they help determine how much energy you have, how well you sleep, your mood and sense of pleasure, and more.
Depression is a complex condition.
The symptoms and severity of depression vary from person to person.
Additionally, while we're gaining a better understanding of how the brain works, we're still discovering new things about mental health every day.
There isn't one single type of scan or test that doctors use when diagnosing someone with clinical depression.
Instead, they rely on multiple tests such as blood tests or CT scans along with patient interviews.
When it comes to brain scans or imaging, doctors usually turn to the following methods:
Each scan provides a different view of the brain — one looks at how the brain is functioning and the other shows which parts of the brain are active — but neither are perfect.
These types of scans have been used to help identify areas of the brain linked to clinical depression, but neither can be used alone to diagnose the disorder.
Brain scans may help physicians identify abnormalities in certain areas of the brain linked to mood disorders like clinical depression, but they do not replace the role of experienced clinicians when it comes to making an initial diagnosis.
Clinical psychologists and psychiatrists both use a well-known tool called the Diagnostic and Statistical Manual (or DSM) to help them diagnose patients with mental health concerns like clinical depression.
The manual provides definitions and examples of symptoms for certain mental illnesses, including clinical depression.
The good news is that even though brain imaging alone isn't perfect for diagnosing clinical depression, it can still be helpful.
In particular, looking at changes over time might help distinguish between people who get better after treatment and those who don't improve as much.
There are a lot of variables that go into diagnosing someone with a mental health disorder.
The idea is that various brain areas are affected in ways we can detect through different kinds of tests.
Some areas may be overactive, while others may be underactive.
A person's serotonin level could be too high or too low—or somewhere in between—and this would affect how they behave emotionally and physically during daily activities.
https://www.nhs.uk/mental-health/conditions/clinical-depression/overview/
https://www.psychiatry.org/patients-families/depression/what-is-depression
https://www.nhs.uk/mental-health/conditions/clinical-depression/causes/
Therapy provides many benefits for people battling depression. Research has shown that cognitive-behavioral therapy (CBT) is particularly effective in managing depressive symptoms. In addition, therapy can teach healthy coping skills and provide emotional support during difficult times. It may also be used as part of a comprehensive treatment plan which includes medication as well as lifestyle changes such as regular exercise and improved nutrition.
While medication is not always required for managing depression, it can be beneficial in some cases. If you decide that medication is right for you, medications such as antidepressants work by balancing certain brain chemicals involved in regulating moods. Other options include mood stabilizers or antipsychotic drugs which may also prove helpful for certain individuals struggling with symptoms of depression.
Yes! In fact, it's encouraged that you open up to your therapist so they can gain deeper insight into your individual situation and develop the most effective treatment plan possible that works best for you. Your therapist is there to serve as an unbiased source of support who will respect any thoughts or feelings shared within the session without judgment or criticism.
The duration of depression counseling varies for each individual, depending on the severity of their depression and their progress in therapy. Our therapists will regularly assess your progress and adjust your treatment plan as needed.
There are many helpful resources available, including support groups, online forums, books and websites dedicated to mental health and wellness. Connecting with other people struggling with the same issue can be especially beneficial. Additionally, talking to a trusted friend or family member can provide much-needed social support during difficult times.
Depression is a mental disorder (a common one) that affects millions of people worldwide. It is characterized by persistent feelings of sadness, hopelessness, and loss of interest in activities once enjoyed.In this section, we will discuss the various types of depression, including major depressive disorder, persistent depressive disorder, and bipolar disorder.Gaining a deeper understanding of your depression is the first step in finding the right treatment and support.