Understanding Client Insurance Benefits
Verification of Benefits usually takes place after the Intake Packet is received or during the Intake phone call. A snippet of what was determined from the client’s benefits can be found when you hover over the appointment.
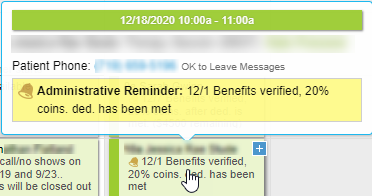
In this example, you can see that on 12/1, benefits were verified, and it was determined that the client’s responsibility is 20% of the fee because the deductible has been met.
Understanding Insurance Terms
What does a copay mean?
- A copay only plan requires that the client pay an exact amount (i.e. $25) for every session no matter the length of the session. 30 - 60 minute psychotherapy sessions will require a copay.
- Copays must be collected by law and cannot be “waived”.
- The deductible is not required to be met on copay plans.
What does coinsurance mean?
- Coinsurance is a percent of the contracted fee of the Provider (i.e. Overcomers Counseling) that is the patient’s responsibility.
- The deductible must be met before the coinsurance split will take effect.
- For example: The client has 20% coinsurance on a Cigna plan, and the deductible has been met. 90837 (60 min psychotherapy session) = $13.60 client’s responsibility
Quoting Insurance Benefits Disclaimer
This disclaimer is used to relay benefit information. This disclaimer is the same disclaimer that the insurance reps use when you call in to verify benefits. Ultimately, the claims department has the final authority when approving/denying claims due to many factors.
This is not a guarantee of benefits and is subject to claim the amount received by your insurance. The patient is responsible for all session fees if the claim is denied for any reason.
Understanding Medicaid Plans
Most Medicaid plans cover mental health services using codes 90791, 90837, 99205, etc. Therapy service codes are billed through the RAE, while medical codes (codes used by NPs) are billed through the Medicaid system.
Family Planning
Clients will occasionally have a "Family Planning" plan with Medicaid. In this case, Medicaid members cannot see outpatient mental health providers (e.g., Overcomers) and must go through their PCP for any mental health services.