Treatment Plan Expectations
Counselors, follow the instructions below on how to write a Treatment Plan. Remember, notes need to be written within 72 hours of DOS. Learn more here: Note Writing Timeliness Policy. Are you tired of writing notes? Use our AI Scribe.
Good Treatment Plan Examples
- Good Sample - Treatment Plan 1.pdf
- Good Sample - Treatment Plan 2.pdf
- Good Sample - Treatment Plan 3.pdf
How to create a Treatment Plan video
Make sure at all times you are using complete sentences, correct grammar, and correct spelling. This is a professional document, and it needs to be written as such. You can use the spell check button at the bottom of the note and download Grammarly to your computer to help you catch grammatical errors.
Clients must sign ALL treatment plans. This can be done via the portal for easy e-signing or in person with clients and then uploaded into their TN file.
Diagnosis
This is automatically populated from the Intake Note.
Presenting Problem
This is automatically populated from the Intake Note.
Treatment Goals
This section must contain 2 items: (1) Client Goal and (2) statement about the client being offered a copy of the TP.
(1) Client Goal
This is best if it is a quote from the client about what they stated their goal(s) are for treatment. Use language similar to - The client wants to…., The client would like to….The client reports their goal for treatment is…..The client and clinician collaboratively created the following goal: ….
Examples:
- Client verbalized the following therapy goals: "I don't want to hurt the people I love anymore, learn to navigate my emotions and heal from my trauma."
- The client would like to “decrease my anxiety so that I can function normally once again.”
- Client and clinician collaboratively developed the following goal: client will utilize her strengths of integrity in order to reduce her symptoms of PTSD to "feel more fulfilled" and feel like she is "growing" and moving forward in life.
(2) A statement about the client being offered a copy of TP.
Examples:
- The client was offered a copy of the treatment plan via the client portal.
- The client was given a copy of the treatment plan in the office.
- The client was offered a copy of her treatment plan and understands that she can access it anytime through the client portal.
The goal must also be specific to treating the symptoms of the diagnosis given. If the client does not give a goal that relates to their diagnosis then it is the clinician’s job to tie the goal into the diagnosis given.
Example:
- Clients stated goal - “Client’s expressed goal is to increase mood and to "get a handle on my mental health, and get back to feeling like myself."
- Clinician ties this into the diagnosis of GAD by stating - “Clinician will aid client in increasing her healthy utilization of coping skills, in order to reduce anxiety."
- So the Goal will read: “Client’s expressed goal is to increase mood and to "get a handle on my mental health, and get back to feeling like myself." Clinician will aid client in increasing her healthy utilization of coping skills, in order to reduce anxiety."
Objectives
There must be a minimum of 2 objectives in each treatment plan.
Each Objective must contain the following 3 items:
- Begin with a strength-based statement
- Include a concrete form of measurement: Sample Concrete Forms of Measurements
- Include a statement about how progress will be measured.
Objectives should be specific to treating the symptoms of the diagnosis given.
Examples:
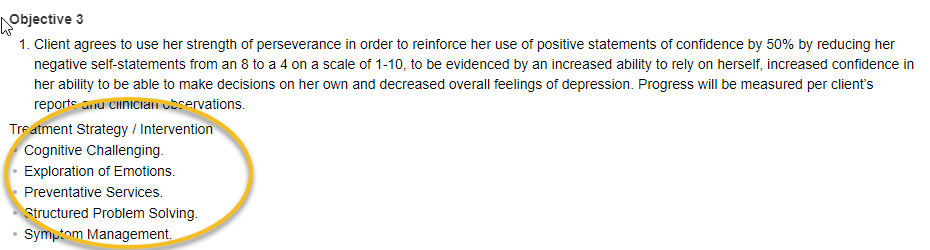
- Client agrees to use her strength of perseverance in order to reinforce her use of positive statements of confidence by 50% by reducing her negative self-statements from an 8 to a 4 on a scale of 1-10, to be evidenced by an increased ability to rely on herself, increased confidence in her ability to be able to make decisions on her own and decreased overall feelings of depression. Progress will be measured per client’s reports and clinician observations.
- The client agrees to use her strength of compassion while challenging negative or anxious thoughts to reduce symptoms of anxiety. The client will implement CBT skills such as challenging, refocusing, and reframing. Progress will be measured by the clinician's observations, as well as the client's self report of her ability to manage anxious thoughts in at least three out of five scenarios.
- The client will use his strength of being motivated for treatment to engage in psychoeducation on the stages of grief to normalize his experience and reduce negative cognitive biases contributing to his sense that he is "crazy". Psychoeducation will occur both in session and through homework assignments to assist the client in gaining skills to decrease his prolonged grief symptoms. Progress will be measured by the clients self report of his ability to challenge, refocus or reframe 2 out of 3 negative cognitive biases identified which contribute to his belief that he is "crazy."
Objective for clients under 12 years old
For clients under the age of 12 there must also be an objective for parents (so you still need 2 for the client and then 1 for the parents - so a total of 3).
Example (for parent/guardian):
- Parents agree to use their strength of love for their son's wellbeing in order to assist him in his treatment goals through bringing the client to his sessions, modeling skills learned during sessions daily, practicing the new techniques at home 2 out of every 3 opportunities that arise, offering supportive statements daily, and being actively involved in his treatment. Progress will be measured per the parent’s self-report.
Treatment Strategy/Intervention - Modality - Frequency - Estimated Completion
This is a new upgrade to TherapyNotes (TN). As seen below TN has provided space under the objective to include treatment strategy/Intervention, Modality, Frequency, and Estimated Completion.
NONE of these fields are “REQUIRED” in TN to be included in your treatment plan (meaning that if you leave them blank, you can still sign the note.
However, OC wants to, at a minimum, see the Treatment Strategy/Interventions you anticipate using with your client during treatment specific to that objective, as seen below (Option 1 Sample):
- You will have to remove (delete) the Modality as TN automatically populates the modality with Individual Therapy
Option 1 Sample (this is the minimum requirement option): Treatment Strategy/interventions added, Modality removed
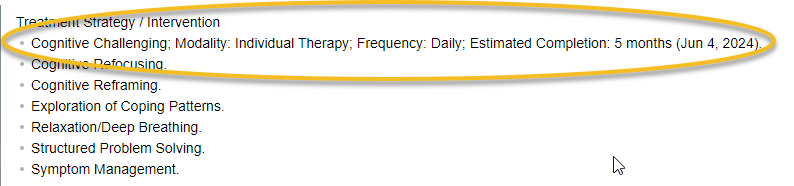
Option 2 Sample: Treatment Strategy/interventions, Modality, Frequency, Est. Complete added
This option which will also be approved by billing supervisors, is to answer the treatment strategy, modality, frequency, and estimated completion one time (in the first row), implying all the interventions will follow suit, as seen below:
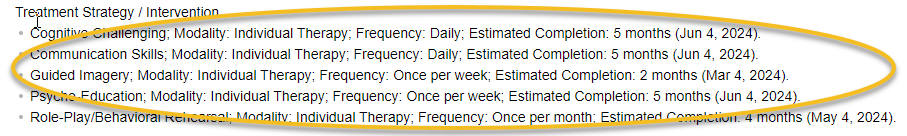
Option 3 Sample: Treatment Strategy/interventions, Modality, Frequency, Est. Complete added on each intervention
This option that will also be approved by billing supervisors is to answer the treatment strategy, modality, frequency, and estimated completion in each row, individualizing each intervention, as seen below:
Discharge Criteria/Planning
Discharge Criteria/Planning - This is what is considered the ultimate way the therapist and the client will know how the clients needs have been met and they are ready to terminate services (discharge). Include the client in writing this goal - how will they know they are done with treatment? A good question you could ask the client to determine what this would be is: "What is your perfect world scenario at the end of treatment? What would that look like for you?" A discharge goal should focus on at least 5 months from now (the point when you would be doing a new TP). This means that it can not be short-term (that is the individual goal). A discharge goal is not required to have a form of measurement in it - it can if that is what you and the client come up with, but it does not have to have a form of measurement. Long-term goals can be changes just like short term goals throughout the course of treatment.
Examples:
- The client will develop alternative responses to substitute for past “coping” choices and make healthy coping choices daily.
- The individual will be capable of identifying appropriate responses to feelings of depression and use them in her daily life, demonstrating management of her depression.
- The client will have developed appropriate substitute self-statements for irrational ones and use them successfully demonstrating increase self-esteem.
- (SUD) The client will establish and maintain total abstinence while increasing knowledge of the substance abuse disorder and the process of recovery.
Additional Information
TN says this section is for “other relevant information if needed, such as strengths or barriers to treatment, supports or other collateral contacts involved in treatment, crisis, relapse, or safety plans, etc.”
- Possible relevant information:
- Including an explanation if the client was given multiple diagnoses and one (or more) of the diagnoses are not going to be included in the treatment between the clinician and the client
- As an example - MDD and Alcohol Use Disorder were both given and the treatment will solely be focused on MDD a statement similar to the following will be included here:
- The clinician has recommended the client seek treatment for their Alcohol Use Disorder through referrals given to them for outside providers that treat SUD diagnoses and engagement in programs such as AA and Smart Recovery.
Prescribed Frequency of Treatment
This needs to be an accurate representation of how often the clinician is recommending the client participate in treatment. If the client will be attending sessions every week then weekly needs to be chosen. This can be edited in every progress note if changes to the frequency are recommended.
Sample Goals/Objectives
Depression
- Client will write in a journal at least 3 times per week as evidenced by self-report.
- Client will spend 5-10 minutes in the sunshine or use a light box at least 3 times per week as evidenced by self-report.
- Client will engage in physical activity, such as walking, for 10 minutes at least 3 times per week as evidenced by self-report.
- Client will leave the house at least 2 times per week for a minimum of 30 minutes as evidenced by client self-report.
- Client will verbalize 3 short-term goals for the future and 2 long-term goals for the future by 4/21/2017 as evidenced by client report in session.
- Client will clarify and verbalize 3 things that make them hopeful in session by 5/20/2017.
- Improve client self-esteem through ability to identify personal strengths in 3 out of 5 opportunities to do so.
Anxiety
- Client will identify at least one cause of stress/anxiety and identify at least two management strategies during weekly therapy.
- Client will practice utilizing the body scan and/or progressive muscle relaxation 4 times per week as evidenced by self-report.
- Client’s score on SMGAD will decrease from 30 to 10.
- Client will utilize deep breathing when feeling precursors of anxiety attack on 3 out of 4 opportunities as evidenced by self-report.
- Client will engage in social interactions with at least 2 individuals outside of immediate family members at least once per week as evidenced by self- and family- verbal report.
- Client will practice deep breathing techniques to mitigate feelings of anxiety in 4 out of 5 opportunities as evidenced by self-report.
- Client will stay in a crowded area for a minimum of 10 minutes, while utilizing coping skills, at least once per month as evidenced by self-report or clinician observation.
- Improve client self-esteem through ability to identify personal strengths in 3 out of 5 opportunities to do so.
Coping Skills
- The client will be able to demonstrate processing of emotions when she is able to utilize 1-3 learned coping mechanisms when escalated.
- The client will learn and implement 1-2 new coping skills per month.
- The client will have the ability to integrate one new coping skill facilitated by this clinician once every 4-6 weeks.
- The client will seek out sensory stimulus to self-soothe when emotionally escalated 2 out of 4 opportunities to do so.
- Integrate developmentally appropriate mindfulness techniques in 3 out of 5 opportunities to do so.
- Client will write in a journal at least 3 times per week as evidenced by self-report.
Emotions/Feelings
- The client will identify cues and symptoms of anger in 4 out of 5 opportunities to do so using skills facilitated by this clinician.
- The client will unpair overwhelming emotions to experience as evidenced by a decrease in 1 to 2 verbal reflections of said overwhelming emotions every 3-4 weeks.
- Client will learn and express feelings verbally versus whining, crying and/or tantrums in 9 out of 12 sessions and 7 out of 10 situations by 5/17/2017, as evidenced by clinician observation and parental report.
- Client will identify and regulate feelings of anger and sadness by communicating with family members and service providers openly and honestly in 9 out of 12 sessions and 7 out of 10 situations by 4/13/2017, evidenced by parental report, client report and clinician observation.
- The client will identify and label feelings relating to trauma in 3 out of 5 opportunities to do so.
- Client will develop anger management skills and use them at minimum twice per week.
- Client will explore emotions and practice appropriate feeling expression skills weekly in session with clinician
- Client will be able to identify 5 emotions in others as evidenced by assessment and observation during session.
Communication
- Youth will work on expressing herself and feeling safe 3 out of 4 opportunities of the time as indicated by behavior and self-report.
- Increase positive communication between client's mother, grandmother and the client by 65% as indicated by verbalizations and active listening by all parties.
- Client will learn 2 appropriate communication techniques and will practice them in session with clinician weekly.
- Client will learn and articulate the pros and cons of poor decisions as they relate to emotional wellbeing and will be able to communicate this understanding effectively in 10 out of 12 sessions and 7 out of 10 situations by 6/14/2017, evidenced by parental report, client report and clinician observation.
- Client will make eye contact with adults while talking in 2 out of 5 opportunities as evidenced by parental report and clinician observation.
Trauma
- The client will repeat and elaborate upon trauma narrative in 3 out of 5 opportunities to do so as a form of desensitization to trauma.
- Repetition of the trauma narrative a minimum of 3 times per month in order to put the event in context within a timeline.
- The client will identify and label feelings relating to trauma in 3 out of 5 opportunities to do so.
- Participate in narrative therapies 1 to 2 times per month.
- Client will explore past trauma and identify how it impacts his life today as evident by 1x weekly identification of a negative effects and a positive change.
Interpersonal/Family
- Family will engage in 1 positive activity together as a family for a minimum of 30 minutes at least once per week as evidenced by family reports.
- Decrease interpersonal issues at home by 50% as indicated by family reports and tracking behaviors.
- Client will identify a minimum of three positive traits of family members and self in 9 out of 12 sessions by 4/13/2017, evidenced by parental report, client report and clinician observation.
- The client will demonstrate increased bond between parents through verbal interactions of feeling expression and/or self-advocacy in 3 out of 5 opportunities to do so.
- The client will demonstrate attachment through appropriate nonverbal exchanges with caregivers in 2 out of 4 opportunities to do so.
- The client will engage in appropriate physical contact with peers and adults in 2 out of 4 opportunities to do so.
- Respond to redirection or response from peers in 3 out of 4 opportunities to do so regarding physical space.
- Demonstrate understanding of boundaries through appropriate response to social settings in 2 out of 4 instances.
- The client will interact with peers appropriately in 2 out of 4 opportunities to do so as characterized by appropriate physical contact and permitting other children to lead play.
- The client will initiate comfort-seeking behaviors in 1 out of 3 opportunities to do so when in a state of emotional dysregulation
- Client will explore with family communication and conflict dynamics to identify and implement strategies to decrease family conflict as evident by reports of successful use of strategies 2x weekly.
- Client and family will be able to express themselves without yelling or arguing at least once per day when talking about or with client.
- Family will utilize “I” statements when discussing family conflict in 3 out of 5 opportunities as evidenced by family reports.
Behavior Management
- Transitions will be healthy and occur easily 3 out of 4 opportunities as indicated by the youth not struggling to physical let go of one individual or “cling” when needing to transition to another caretaker.
- Client will be able to identify consequences related to triggers and will be able to communicate these consequences effectively in 9 out of 12 sessions and 7 out of 10 situations by 5/19/2017, evidenced by parental report, client report and clinician observation.
- The client will participate in behavior mapping in order to improve behaviors in structured settings as evidenced by ability to control impulses in 2 out of 4 opportunities to do so.
- The client will urinate in appropriate settings as a bodily function in 9 out of 10 opportunities to do so.
- Respond to redirection or response from peers in 3 out of 4 opportunities to do so regarding physical space.
- Demonstrate understanding of boundaries through appropriate response to social settings in 2 out of 4 instances.
- The client will implement skills used in social stories in 3 out of 5 opportunities to do so.
- Client will stop and think for a minimum of 10 seconds prior to making a decision at minimum twice per day.
- Client will take accountability for his actions 8 out of 10 times as evidenced by self and family reports.
- Client will place hands in pockets when prompted 2 out of 5 times as evidenced by parental report.
- Client will hand toys nicely to peers, instead of throwing, in 2 out of 3 opportunities as evidenced by parental report.
Play
- This clinician will guide the implementation imagination play in session and the client will participate in this type of play in 2-3 sessions per month.
Interventions
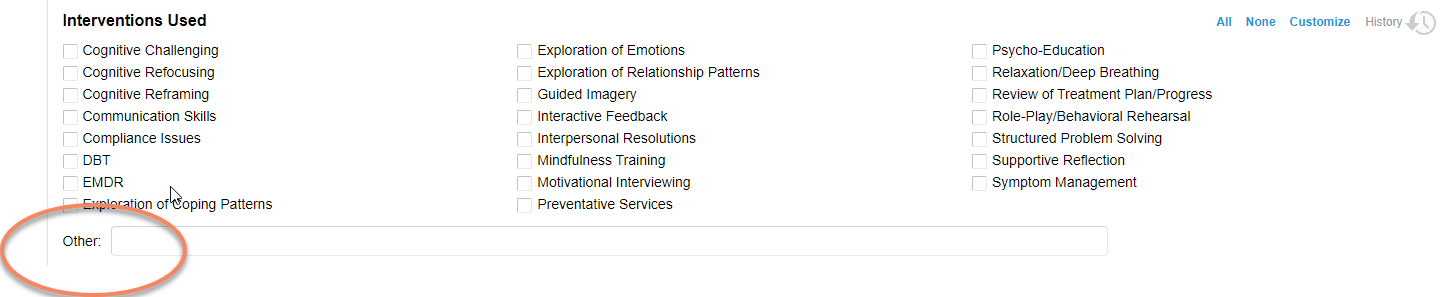
Interventions used with clients
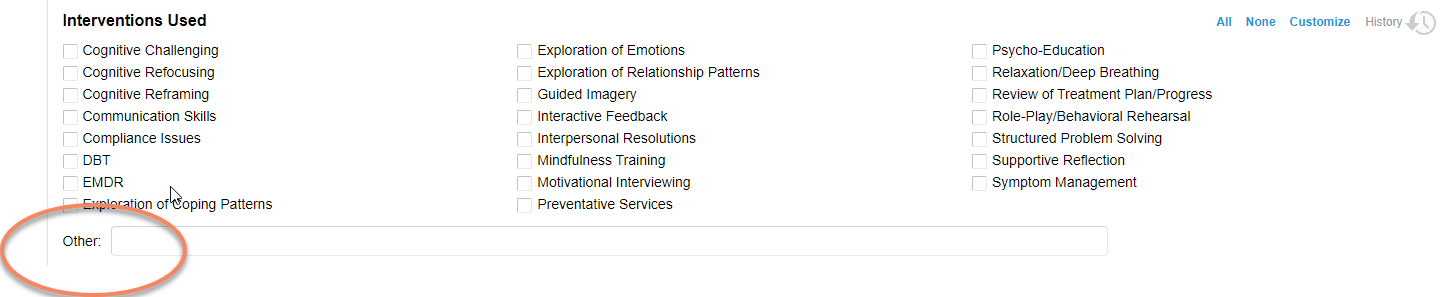
You do not have to only use the interventions TherapyNotes gives you in the Interventions used section which are:
- Cognitive Challenging, Cognitive Refocusing, Cognitive Reframing, Communication Skills, Compliance Issues, DBT, EMDR, Exploration of Coping Patterns, Exploration of Emotions, Exploration of Relationship Patterns, Guided Imagery, Interactive Feedback, Interpersonal Resolutions, Mindfulness Training, Motivational Interviewing, Preventative Services, Psycho-Education, Relaxation/Deep Breathing, Review of Treatment Plan/Progress, Role-Play/Behavioral Rehearsal, Structured Problem Solving, Supportive Reflection, and Symptom Management.
You can add any interventions you use with clients into the “Other” box.
Here are some examples of other interventions you may be using with clients during your sessions:
- Miracle question
- Open-ended questions
- Appropriate use of silence
- Paraphrasing
- Reflection, Reflecting back
- Summarizing
- Acknowledgment
- Empty chair
- Focusing on repressed emotions
- Exploration of decision making
- Building self-efficacy
- Enhancing self confidence
- Positive visualization
- Taking an inventory
- Exploration of triggers, identifying triggers
- Modeling acceptance
- Transforming troublesome thought patterns
- Deconstruct harmful thought patterns
- Breaking negative connections
- Journaling to track behaviors/thoughts/actions,etc
- Encouraging a more positive mindset
- Meditation
- Reinforcement
- Operant conditioning
- Identifying maladaptive beliefs
- Processing traumatic memories
- Gradual exposure
- Taught behavior management techniques
- Teaching self-regulatory skills
- Paradoxal Interventions
- Behavior Reinforcement
- Anger management
- Collaborative Problem-Solving
- Labeling feelings
- Stress management
You may be doing the following types of therapy with clients that can be added to the “Other” box as well:
- Dance/Movement Therapy
- Play Therapy
- Art Therapy
- Laughter Therapy
- Drama Therapy
- Music Therapy
- Positive Psychology
- Brain Spotting
- EFT
- Gottman Couples Counseling Techniques
- Sandplay
Descriptive Intervention Words
- Asked
- Assisted client in
- Acknowledged
- Affirmed
- Challenged
- Clarified
- Coached
- Collaborated
- De-escalated
- Demonstrated
- Developed
- Directed
- Discussed
- Encouraged
- Explained
- Examined
- Explored
- Evaluated
- Facilitated
- Focused on
- Gave homework
- Guided
- Instructed
- Interpreted
- Introduced
- Inquired about
- Listened
- Paraphrased
- Performed
- Planned
- Practiced
- Praised
- Prompted
- Provided
- Redirected
- Reflected back
- Reframed
- Refocused
- Reinforced
- Responded to
- Reviewed
- Role played
- Set boundaries
- Shared
- Supported
- Trained
- Validated
Couples/Family TP
In the treatment plan the goals and objectives will be written for the “client” which is the individual on the TN file. For example:
Treatment Goal Example
Client stated that her goal for counseling is to process the conflict she is experiencing in her relationship with her spouse that is causing her anxiety symptoms and have a unified vision with her spouse moving forward about investing and their careers. The clinician will teach the client CBT skills that will assist her in decreasing tension in the marriage.
Objective #1
Client agrees to use her strengths of joy and drive to help her learn 3-5 new communication tools and skills to be used at a minimum of 1-3 times daily during conversations that take place between the client and her spouse in order to help her to communicate and engage in conflict in a healthy way with her spouse. Progress will be monitored via counselor observation and client report in session.
Objective #2
Client agrees to use her strength of perseverance in order to understand the role that cognitive biases play in excessive irrational worry and persistent anxiety symptoms and replace 1-3 potential biases such as the probability of the negative expectation occurring, the real consequences of it occurring, and her ability to control the outcome with realistic thoughts to decrease her anxiety and increase her ability to accept it which will in turn aid in the client’s ability to connect with her spouse. The client will be able to report a decrease in her anxiety from an 8 to a 5 on a scale of 1-10 with 10 being intense anxiety and 1 being no anxiety. Progress will be measured per (client’s name) self-reports and clinician observations.
Discharge Criteria/Planning
The discharge goal is as follows: The client will be able to report marital satisfaction at a 9 on a scale of 1-10 with 10 being completely satisfied.
Sample Couples TP
Diagnosis
F43.21
Adjustment Disorder, With depressed mood
Z63.0
Relationship Distress with Spouse or Intimate Partner
The client experiences emotional and behavioral symptoms (worry, low affect, conflict, withdrawal) as a result of an identifiable stressor (spouse desire for seperation). These symptoms began within 3 months of the onset of the stressor and significantly impact the clients ability to function in social and other important areas of functioning.
Presenting Problem
The client reports a marriage of 15 years with frequent periods of disruption and discontent. The client reports difficulty with communication and conflict management throughout their relationship. The client reports his wife has been emotionally disconnected and disengaged from the relationship since approximately sept 2021 and is now considering pursuing divorce. The client reports he has been working with an individual counselor to overcome many of the challenges that were barriers in the relationship; however, the client reports his spouse "walled off" and no longer vulnerable or emotionally open within the relationship. The client reports a desire to improve communication and understanding in the relationship, as well as explore whether they can repair the marriage.
Treatment Goals
The client states his goal for counseling is to improve his ability to communicate and resolve conflict with his spouse as well as increase emotional intimacy and trust. The clinician will use the Gottman method and teach skills to improve the client's ability to communicate and connect with his spouse.
The client was offered a copy of the treatment plan.
Estimated Completion: 5 Months
Objective #1
The client will use his strength of commitment to learn interpersonal communication skills including softened start-up, repair attempts, self-soothing, and compromise. The client will receive psychoeducation based on identifying and eliminating Gottman's 4 horsemen; criticism, contempt, defensiveness, and stonewalling. Progress will be measured based on the clinician's observations and self-report of successful communication in 3 out of every 4 attempts.
Treatment Strategy / Interventions: Exploration of Emotions, Exploration of Relationship Patterns, Exploration of Coping Patterns, Psycho-Education, Communication Skills, Socratic Questioning, Supportive Reflection, Relaxation/Deep Breathing
Estimated Completion: 5 Months
Objective #2
The client will use his strength of familiarity and knowledge of his spouse to expand "love maps", nurture the fondness and admiration for his spouse, increase turning towards each other and creating openings, and creating shared meaning. Progress will be measured by the client's self-report of relationship health, connectedness, and satisfaction using 1-10 scaling questions (with 1 being low and 10 being high) with a goal of 7.
Treatment Strategy / Interventions: Exploration of Emotions, Exploration of Relationship Patterns, Interactive Feedback, Interpersonal Resolutions, Supportive Reflection, Socratic Questioning, Communication Skills
Estimated Completion: 5 Months
Discharge Criteria/Planning
The discharge goal is to increase the client's report of marital satisfaction to 8 on a scale of 1 (low) - 10 (complete satisfaction).
Additional Information
The client’s husband is currently reluctant to participate in couples counseling which may hinder the client’s abilities to reach treatment goals and objectives.
Prescribed Frequency of Treatment
Weekly
I declare that these services are medically necessary and appropriate to the recipient's diagnosis and needs.
Signed TPs
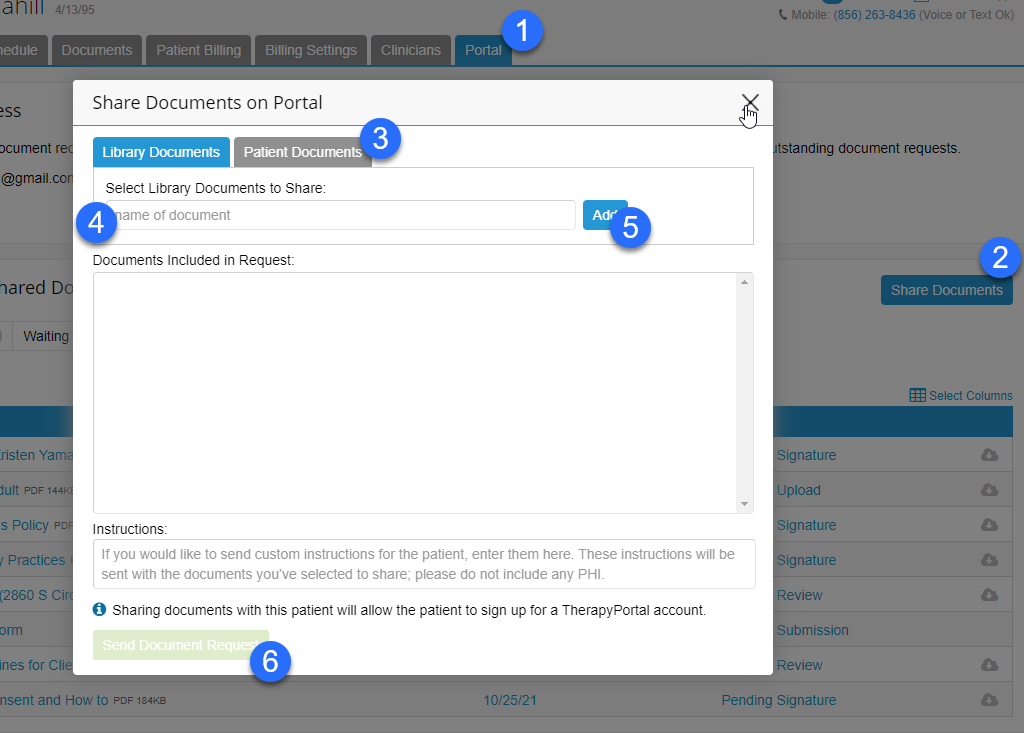
Treatment plans must be signed by the client for both the initial treatment plan and all subsequent treatment plan reviews. This can be done either in person with the client or via the portal. If you have the client sign the TP in person then you will want to scan the document and upload it into their file. If you are doing teletherapy (or you just prefer this method) you can add their TP to the portal and they can e-sign the document.
To send a client a treatment plan for signature, send it through the client portal.
Go to the client in TN >> Portal tab >> Share Documents button >> Patient Documents >> in the name of the document start typing “treatment” >> set to “E-Sign” >> click “Send Document”.
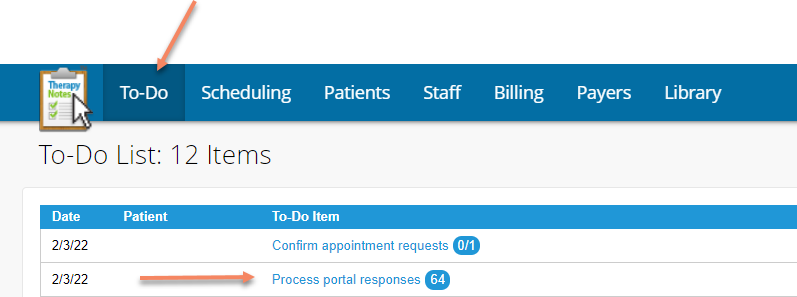
See who signed the TP
- Go to your To-Do tab.
- Click on Process Portal responses If you don’t have “process portal responses,” go here:
- Click on Custom
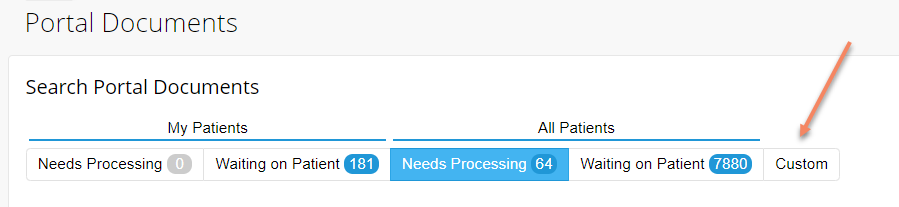
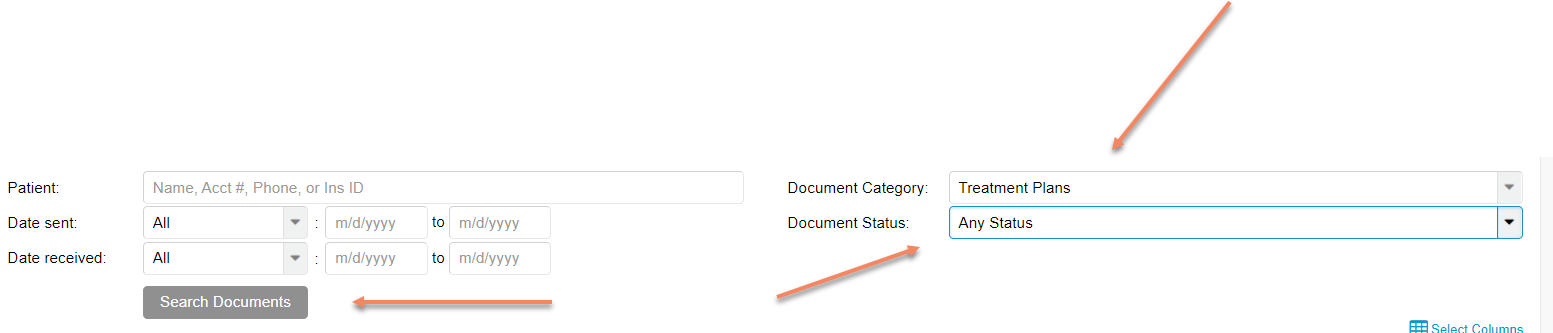
- Choose from the drop-down menu: Document Category - Treatment Plans, Document Status - Any Status. Then click Search Documents.
- See the status of the TP (Pending Signature, Viewed Pending Signature, Needs processing, Signed on (date).

Updating a TP at 150-180 days
When the clinician created the original treatment plan, the estimated completion time was marked at 5 months. At 150 days (5 months), TN will create a To-Do Item in your To-Do tab. At 180 days, the clinician will not be allowed to write a progress note until the treatment plan is updated (this is an insurance requirement).
Steps to update a TP
DO NOT “edit” an old TP!
- Click on the above blue “Create a new Treatment Plan since the most recent Treatment Plan is more than 150 days old.” (Or you can create a new TP in Documents - Create Note - Psychotherapy Treatment Plan)
- The previous treatment plan will be opened up.
- From here you can:
- Update the diagnosis (if needed)
- Change/update the treatment goal
- Be sure to that the following statement is in the goal section: The client was offered a copy of the treatment plan (you can state - via the client portal if that applies).
- Change/update the objectives
- Change/update the discharge Criteria/Planning statement
- Sign the updated TP
- Save
- Send updated TP via the portal (or get it signed in person).
Do NOT open and change the previously saved TP. Instead, create a new TP or click on the To-Do mentioned above, stating “Create a new Treatment Plan…”. If you go in and change/edit the original TP the date will change, and the original TP will be lost. This will cause the client’s file to appear as if a TP was never written prior to the most recent TP, which will present problems during audits where we need to show updated TPs every 6 months.
How to update a TP
- Take time during the next session to review the current TP with the client and determine the next steps of treatment (will the treatment plan stay the same, require some modifications, or are all new objectives necessary as old objectives have all been met, etc).
- In the Treatment Goal section add a statement under the current goal similar to:
- *Update - 1/1/22 - Clinician and client reviewed the current treatment plan and have made updates to the objectives to reflect the current treatment needs.
- *Update - 1/1/22 - The client reports a desire to keep the TP as is at this time due to her only being seen monthly and reporting that she is still working toward mastery of these goals.
- If updated objectives are needed there are two ways to make changes:
- You can just make the necessary changes to the current objective. For example:
- Original Objective 1: Client agrees to use her strengths of being brave and courageous, to learn and use 1-5 coping skills (at a minimum of 1 time daily) such as breathing, grounding, etc. to reduce her symptoms from a 7-8 to a 3-4 on the scale noted above. Progress will be measured per client's reports and clinician observations
- Updated Objective 1: Client agrees to use her strengths of being brave and courageous, to learn and use 3-7 coping skills (at a minimum of 3 times daily) such as breathing, grounding, etc. to reduce her symptoms from a 5-6 to a 2-3 on the scale noted above. Progress will be measured per client's reports and clinician observations
- You can remove an objective that has been completed or the client no longer is working toward and replace it with a more current objective.
- You can just make the necessary changes to the current objective. For example:
- Reminders:
- The goal can either be a client quote, or use language similar to “The client wants to, would like to, desires to,” etc. in order to demonstrate the client participated in creating the goal.
- Be sure that the goal includes a Long Term Goal (AKA Discharge Goal) - This is what is considered the ultimate way the therapist and the client will know how the clients needs have been met and they are ready to terminate services (discharge). Include the client in writing this goal - how will they know they are done with treatment?
- Be sure to that the following statement is in the goal section:
- The client was offered a copy of the treatment plan (you can state - via the client portal if that applies)
- There must be at least 2 objectives (3 if the client is a minor, one of which is for the parent/guardian)
- Objectives must contain these 3 components:
- A strength based statement
- A form of measurement (can not be vague - decrease by 50%)
- How progress will be tracked
- Set the Estimated Completion at 5 months for the goal and all objectives.
- TP must be signed by the client (via portal or in person and then uploaded to the file)
Updating a TP before 180 days
There are several reasons you may need to update a TP before the 180-day requirement is met. Those could be situations such as:
- Initially, the client was assigned a diagnosis of F99 because the clinician required additional time to determine the appropriate and accurate diagnosis.
- During treatment, the client experiences an event that would necessitate a new or additional diagnosis.
- Example: Client experiences the traumatic event of losing their child and is now experiencing trauma-related symptoms (PTSD, Acute Stress, Unspecified Trauma and Stressor-Related Disorder)
- During treatment, the clinician determines that the client meets the criteria for an additional diagnosis.
Steps to update a treatment plan before 180 days
- In the progress note for the most recent session, the clinician writes in the plan section that the client’s diagnosis will be updated to reflect the current accurate diagnosis (this could also be written in the objective content section as something the clinician and the client discussed during the session).
- At the bottom of the progress note for the Recommendation, choose: change treatment goals or objectives.
- A To-Do will populate:
- Create a new Treatment Plan to reflect recent changes in diagnosis or treatment objectives.
- Create the new TP and add the correct/new diagnosis
- Do not forget to modify the goals/objectives to reflect the new appropriate diagnosis.
- If necessary, update the Discharge Criteria/Planning - This is what is considered the ultimate way the therapist and the client will know how the client's needs have been met and they are ready to terminate services (discharge). Include the client in writing this goal - how will they know they are done with treatment?
- Be sure that the following statement is in the goal section:
- The client was offered a copy of the treatment plan (you can state - via the client portal if that applies)
When updating a TP at the 5-month mark (or sooner), DO NOT go in and change the previously saved TP. Instead, create a new TP or click on the To-Do mentioned above stating “Create a new Treatment Plan…”. If you go in and change/edit the original TP the date will change, and the original TP will be lost. This will cause the client’s file to look like a TP was never written prior to the newest TP, which will present problems in an audit where we need to show updated TPs every 6 months.
Updating a TP and writing a Progress Note the Same Day
When you update a TP the same day that you need to write a progress note (in the example of updating a TP at 150 days for a client who is continuing treatment) in the treatment plan you need to change the time the note is written to at least 5 minutes before the session took place. So for example, if the session is to start at 1pm set the TP time as 12:55pm and then it will populate into the progress note with the updated TP information.
Here are the steps:
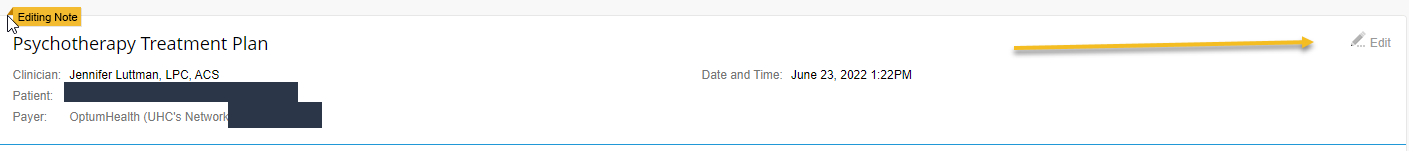
- In the TP click on the edit button in the upper-right corner:
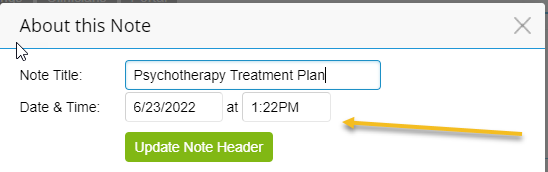
- Change the time to be at least 5 minutes before the session start time:
TP Planners
Find helpful note samples/guides/text on our Google Drive: Shared Drive >> Therapy Resources >> Psychotherapy Planners.
TP Requirements
Treatment Plans must be signed by clients every time. You can upload them to the portal for quick e-signing by the client. Treatment Plans must be updated every 180 days. The updated Treatment Plan must be signed again by the client.
General Reminders about TP
When writing a treatment goal it is best practice to ask the client what their treatment goals are and then use that verbiage - and put it in quotes - for the treatment goal. This demonstrates to the reader that the client was an active participant in creating the treatment plan. For example, you could say - The client verbalized their goals for treatment were to "learn how to cope with my sadness better," or The client verbalized their goal was to "learn how to cope with the ongoing stress in my family life."
- There must be at least 2 objectives in every treatment plan. (3 for minor clients)
- Objectives must be measurable and note how progress will be tracked. Measurements can look like using a 1-10 scale, 1 out of every 3 times, twice a week, as a few examples. Tracking progress can look like - as evidenced by, through client self-report, journaling that will be shared in each session, etc.