T1017 Consultation Note
T1017 is targeted case management (8-15 minutes per unit) for Medicaid clients only.
T1017 Service Code Description:
Services designed to assist and support a patient diagnosed with or being assessed for a mental health disorder to gain access to needed medical, social, educational, and other services, as well as provide care coordination and care transition services, including:
- Assessing service needs – gathering patient history/collateral info, treatment needs;
- Treatment/Service plan development – specifying goals and actions to address patient needs, ensuring participation, identifying a course of action; includes transition plan development
- Referral and related activities to obtain needed services – arranging initial appointments for patient with service providers/informing patient of services and/providing contact information for available services; working with patient/collaterals to secure access to services, including contacting agencies for appointments/services after initial referral process; and
- Monitoring and follow-up – contacting patient/others to ensure patient is following the agreed upon service or transition plan and monitoring progress and impact of plan.
Minimum Documentation Requirements:
- The reason for the visit/call. What was the intended goal or agenda? How does the service relate to the treatment/service plan?
- Description of the service provided (specify issues addressed (adult living skills, family, income/ support, legal, medication, educational, housing, interpersonal, medical/dental, vocational, other basic resources)
- The services utilized and the individual’s response to the services (includes assessing service needs, treatment/service plan development, referral, and monitoring/follow-up, which includes care coordination)
- How did the service impact the individual’s progress towards goals/objectives?
- Plan for next contact(s) including any follow-up or coordination needed with 3rd parties
Example Activities:
- Assessing the need for service, identifying and investigating available resources, explaining options to patients and assisting in the application process.
- Contact the patient’s family members for assistance in helping the patient access services.
- Care Coordination between other service agencies or healthcare providers.
- Development and follow-up of a transition plan from the hospital to outpatient services.
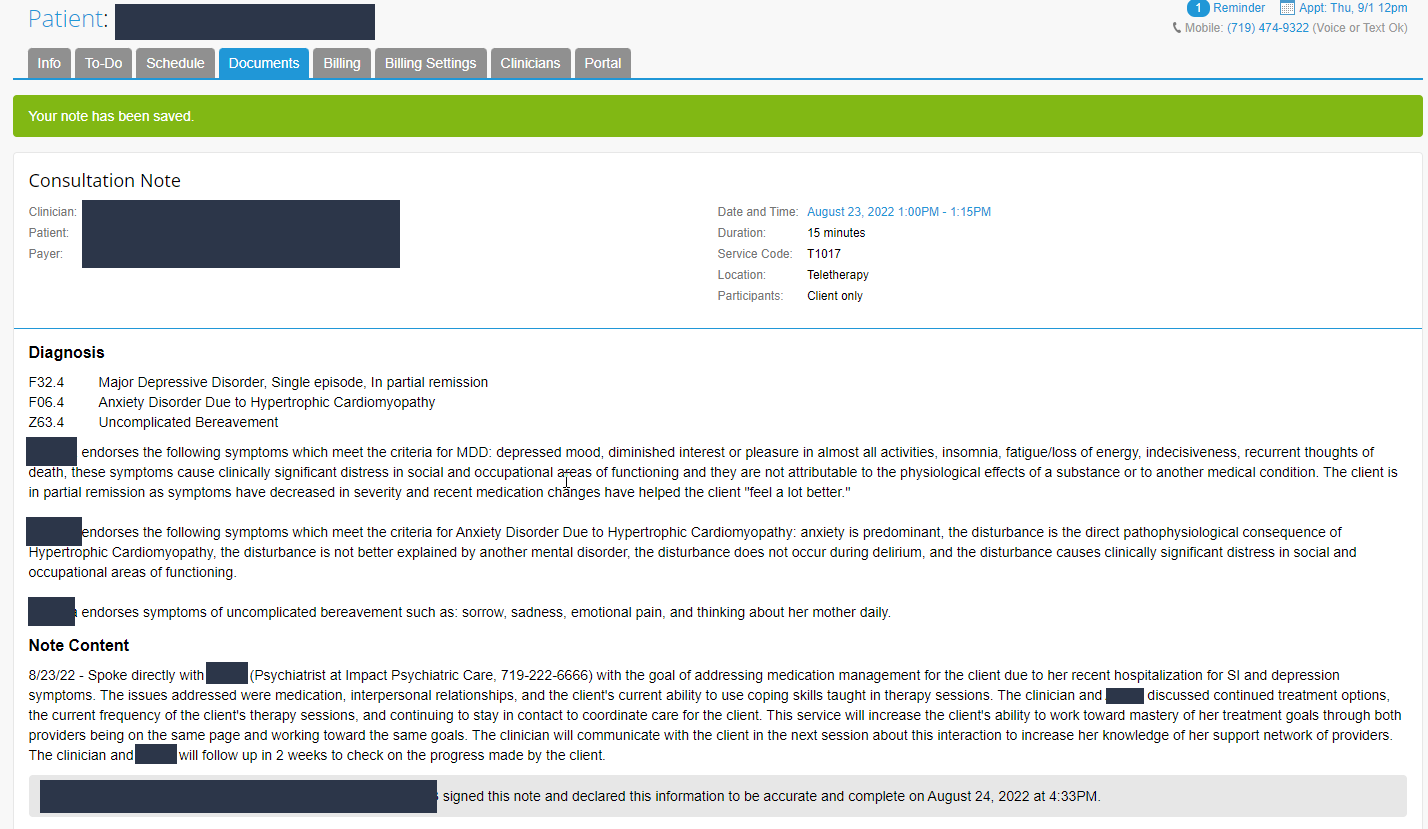
Billing This Code
Learn more here: Billing the Service Code T1017