SI Cheat Sheet
Are you tired of writing notes? Use our AI Scribe.
Step 1: Conduct an Assessment
Any time a client reports they have experienced suicidal ideation (even passive suicidal ideation) an assessment must be conducted.
Assessment Options:
- Preferred Method: Go to the client’s file in TN >> Portal tab >> click Share Documents >> search for the C-SSRS: Columbia-Suicide Severity Rating Scale (Screener, Recent) outcome measure and send it. There is also a clinician-administered C-SSRS that can be used by the clinician during the session.
- Alternative Method: Download one of these docs: ASQ.pdf or Columbia Short Version.pdf. After completing the PDF, upload it to the client’s file in TN.
Step 2: Create a Safety Plan
If the client has a positive screen for SI or HI, you must create a safety plan (and document the safety plan in the additional details box of the note for the session during which the SI was discussed). A safety plan must also be written if the client has been hospitalized in the last 90 days. This should ideally be created during the same session. If that is not possible (maybe due to time constraints), a statement must be made in the note that a safety plan will be written with the client in the next session.
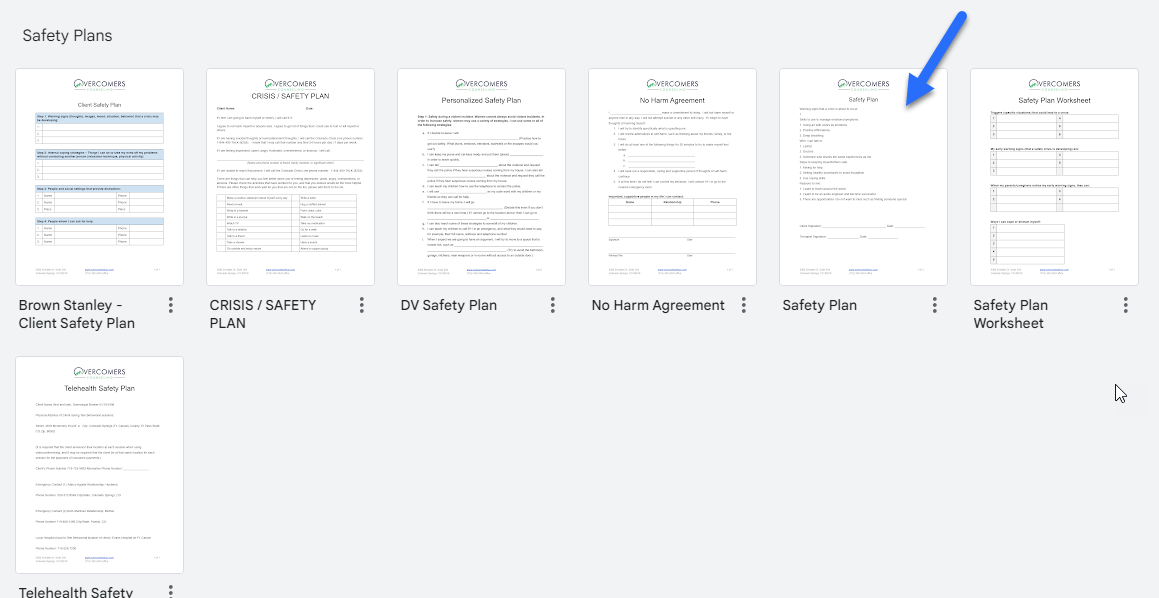
Options to Create a Safety Plan
You can create a safety plan by using Heidi AI, sending the form via the Portal, or via our Template Gallery.
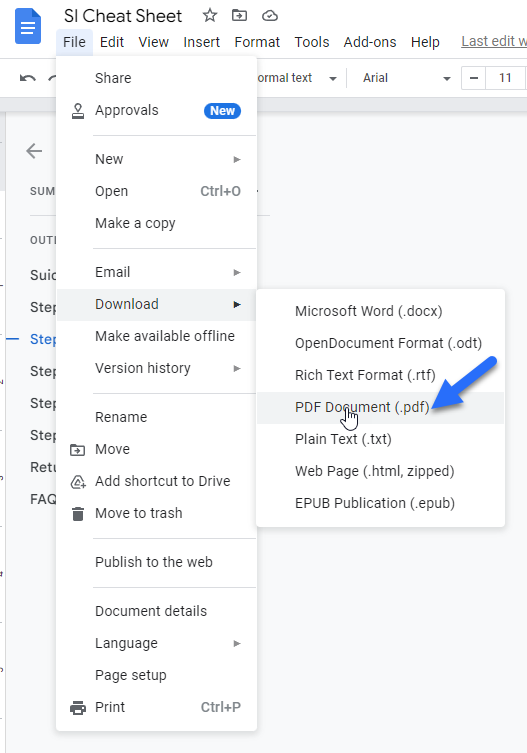
- Use Heidi Health AI Scribe: Use the Heidi Health AI Template called “OC Brown Stanley - Safety Plan”. Once created, export from Heidi Health into a PDF. How to use Heidi Health (AI Scribe).
- Use TN Library: Send the "Safety Plan" portal form to the Client Portal. The client will complete the form; however, you can help them fill it out.
- Use Template Gallery: Sample Safety Plans can be found in our Template Gallery. Once you create the Safety Plan document, download it as a PDF to upload to the Client Portal.
The Client must sign the Safety Plan
Safety Plans must be signed by the client (in person or sent over the portal for signature) and added to their file.
Step 3: Provide the Client with Crisis Information
Every time a client expresses SI (even passive), we need to share/remind the client of the crisis resources.
The note (intake or progress note) needs to state that the clinician provided the client with emergency/crisis information or that it was reviewed.
The crisis information can be found on your disclosure statement. Here is a link to the information on our website: Crisis Information. The Safety Plan form also includes some crisis information.
Step 4: Following sessions (after initial SI was reported)
- For any client who has been hospitalized or had an actual attempt, an assessment must be done for 90 days after the hospitalization or attempt. The reason for this is that attempts after hospitalization are 300 times more likely in the first week and 200 times more likely in the first 90 days after release.
- For any client who has reported SI and an assessment has been done the clinician needs to continue to do an assessment at each session for (at a minimum) one month (4 sessions) of the client responding no to all questions (except for SI within the past month). If the client continues to report SI then continue doing the assessment at each session until no is the answer to all questions for one month.
- Upload the assessment each time it is completed to the client’s file.
- Each time you do an assessment review the safety plan to ensure it is still accurate and meets the client’s needs and if not make adjustments and get a new signature from the client on the updated safety plan. Document this review of the safety plan in the progress note in the safety risk section.
Step 5: When a referral to a higher level of care is necessary
If you have determined that a client is high risk and needs to be either taken or transported to a higher level of care you must stay with the client (either in person or virtually) until the person who is taking them has arrived or medical professionals have arrived to transport the client. Do not ever leave a client or end a session with a client in crisis without confirming the client has transportation to the emergency room/hospital.
If, when giving an assessment or before the assessment, it is determined that the client needs a higher level of care, such as being taken to a formal evaluation at a hospital or crisis center, you have two options:
- Option 1 - Send the client on their own (or have a parent/guardian/friend) take them to the hospital
- It is best practice to call ahead and notify the location the client will be going that they are coming and give them your recommendation in regards to their safety concerns.
- Ask the driver (client or person taking them) to contact you once they have arrived.
- Make a follow-up contact attempt the following day unless you know that the client has been placed on a 72-hour hold, and then reach out at the end of the 72-hour hold to make contact and schedule a future session.
- Document these contacts in your note (intake or progress or contact note).
- Option 2 - M1 Hold - *Only LICENSED clinicians can write an M1 hold. If you are not licensed, call the police for an M1 hold.
- As an alternative option - Candidates (unlicensed therapists) may refer a client presenting with this level of risk to their supervisor, and a hold can be implemented by the Supervisor.
- If the client is unable or unwilling to commit themselves for assessment then you can call AMR or Local Police in order to have the police or the ambulance come and transport the client to a local hospital.
- Jamaica Office only - Call Aurora Police Crisis Response Team, 303-627-3100
- AMR phone number: 719-597-1277 (Colorado Springs), 719-545-1226 (Pueblo), 303-357-2000 (Aurora)
- Police: 911
- Fill out the M1 hold paperwork here: COLORADO MENTAL HEALTH M-1-FORM.pdf
- For Colorado Springs, you can email a copy of the M1 hold to AMR here: amr.co.springs@amr.net
- For Pueblo and Aurora, when you call AMR, ask where you can email the M1 hold.
- Wait with the client until the police or AMR shows up, answer any questions they have and give them a copy of the M1 hold.
- Add a copy of the M1 hold to the client’s file.
Returning to outpatient treatment after a hold or inpatient care
- If, upon exiting a hold or inpatient care, it is determined that individual therapy is not the appropriate placement for the client due to their high risk and to provide sufficient care to address their safety concerns, partial hospitalization or IOP should also be considered.
- If it is determined that individual therapy is the appropriate treatment approach, assess to determine if weekly sessions or twice-a-week sessions are appropriate for the client.
- In-person sessions are best practice with clients who are at high risk for SI.
FAQ
What if my in-person client runs out of the office or my teletherapy client ends the session?
- Contact Emergency Contact Person (intake questionnaire) - A specific plan is laid out in the consent form that all teletherapy clinicians have their clients’ consent to reach out to an emergency contact to confirm safety if, for any reason, they are disconnected.
- If you have determined the client is a risk to themselves or you think they might be you need to call 911 and report what took place and the reason you are concerned for your client’s safety. You are calling for a welfare check on your client. You will need to provide the last known location of the client and their home address (in their file) and answer any questions the 911 operator may have for you.
What if I have an ongoing crisis client via telehealth?
- If the client demonstrates an ongoing crisis (active SI—including plan and intent for 2+ sessions), the client should be referred to either in-person services or a higher level of care.