Progress Note Expectations
Counselors, follow the instructions below on how to write a Progress Note. Remember, notes need to be written within 72 hours of DOS. Learn more here: Note Writing Timeliness Policy. Are you tired of writing notes? Use our AI Scribe.
Good Example:
How to create a Progress Note video
Make sure at all times that you are using complete sentences, correct grammar, and correct spelling. This is a professional document, and it needs to be written as such. You can use the spell check button at the bottom of the note and download Grammarly to your computer to help you catch grammatical errors.
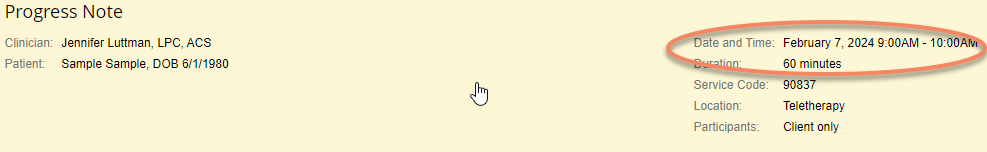
Note Header
The below image is a sample Progress Note Header unchanged by the clinician (auto populated by TN):
(90837, 60 minutes, 9:00am - 10:00am)
Insurance wants to see the actual Face-to-Face time put in this note header, not the auto-populated information.
(In the note header, click on the “Edit” button and adust the time in the white box that appears).
The below image is a sample Progress Note Header that has been changed by the clinician to reflect the actual fact to face time they spent with the client:
(90837, 53 minutes, 9:10am - 10:03am)
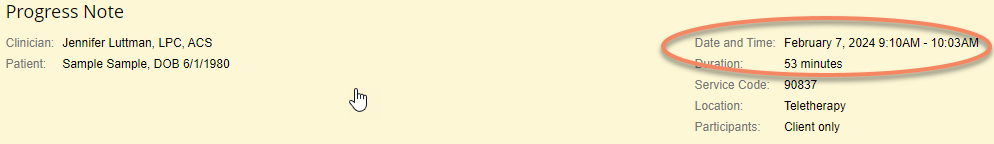
The time could start early, start on time, start late, end early, end on time, or end late - any of these are allowable and are what insurance wants to see as far as the “Duration” of the session goes.
- For 90837 - the duration must be between 53-60+ minutes
- For 90834 - the duration must be between 38-52 minutes
- For 90832 - the duration must be between 16-37 minutes
Diagnosis
This is automatically populated from the Intake Note.
Current Mental Status
You can check “all normal” and then modify according to what the client presents as in the session.
Example:
For a depressed client, you would want to change their mood from Euthymic to Depressed, or change their Affect from Congruent to Flat, etc.
Risk Assessment
Check the box - Client denies all areas of risk. No contrary clinical indications present - if the client reports no risks. If the client is reporting risks then include the area of risk, the level of risk, intent to act, plan to act, means to act, risk factors, and protective factors.
If the client is reporting risks (within the past 30 days to present) then include the area of risk, the level of risk, intent to act, plan to act, means to act, risk factors, and protective factors.
3 required steps:
- Conduct a risk assessment - ASQ or Columbia
- The risk assessment must be uploaded to the TN file (and documented in the additional details box)
- If the client tests positive for SI or HI, you must create a safety plan and document it in the additional details box. If the client has been hospitalized in the last 90 days, a safety plan must also be written.
- The safety plan must be uploaded to the TN file and must be signed by the client.
- This can be sent via the portal for e-signing or signed in person and uploaded.
- In addition, we must review emergency/crisis information with the client (and document this review in the additional details box)
Medications
Include any medications the client is currently prescribed. If no changes have taken place from the previous note you can write “No medication changes were reported by the client.”
Example:
Client reported that she is prescribed Adderall by Dr. Jenny Storms through Mastermind Clinic and had just started Lamictal after several evaluative sessions with her doctor as she has been diagnosed with Bipolar II.
Symptom Description and Subjective Report
The symptom description is the section where you must demonstrate medical necessity by reporting the client’s symptoms. The subjective report is where the therapist shares their observations of the client and their perceptions of the client.
Demonstrate medical necessity by having the client answer these questions:
- Symptoms of their diagnosis since the last session
- Duration of the symptoms since the last session (minutes, hours, all day every day, off and on, etc.)
- Frequency of symptoms since the last session (daily, every other day, more days than not, etc.)
- Severity of the symptoms since the last session (mild, moderate, severe) (Likert scale)
- Impairment/impact on functioning since the last session
If the session was a teletherapy, you must include a statement about the client’s location and ability to speak freely/confidentially during the session.
How would you describe it as teletherapy?
- This session was conducted via teletherapy.
- The session was held via teletherapy per the client's request.
- The therapy session was conducted between the therapist and the client using Client Portal video chat software.
How would you describe the client's location?
- The client confirmed that she was located in her mother's office and she confirmed that she had privacy and could talk freely.
- The client reported their location was in their home and they reported sufficient privacy to conduct a teletherapy session.
Examples:
- The client reports the following symptoms over the past week; fear that prevents her from leaving her home, freezing when she needs to leave the home, racing heart, sweaty palms, difficulty breathing, irrational thoughts about something bad happening to her if she leaves the house, anxiety, and worry. The client reports that her feelings of fear and “feeling frozen” occurred for a duration of 1 hour each time they happened. She states that she has experienced the above-mentioned symptoms at a frequency of 3-4 times this past week. The client’s symptoms are reflective of moderate severity due to the impact they are having on her weekly. The client reports that she was unable to go to work for three days this week due to her panic symptoms and her inability to get in the car and drive to work. She was open to discussing and processing these feelings and situations with the therapist. She reported the ability to practice healthy self-care through maintaining a positive support system with her friends and close family members. She continues to explore the root causes contributing to symptoms of anxiety, panic, and self-doubt. The session was conducted via teletherapy and the client confirmed that he was located in his mother's office and he confirmed that he had privacy and could talk freely.
- The client endorsed experiencing depressive symptoms such as depressed mood, lack of motivation, sleep difficulties, sadness, racing thoughts, intrusive thoughts, shame, and low self-esteem about half of the days (3 out of 7) for the majority of each of those days, since the last therapy session. The client further endorsed experiencing trauma-related symptoms such as unwanted memories of past childhood traumatic events, shame, intrusive thoughts, numbness, irritability, feeling checked out, and being easily startled for 5 out of the past 7 days for about 3 hours per day. The severity of the client’s symptoms over the past week appeares to be moderate due to the impact it is having on his ability to engage in work fully and the continued impairment he is experiencing in his personal relationships. The client reported being more mindful of the negative internal dialogue he has and explored how this relates to his past abuse and neglect (which does not need to be reported as the perpetrators are deceased). The client began to gain insight as evidenced by the client stating, "I think those critical thoughts aren't mine but my parents." The client endorsed being able to feel more positive emotions in the past week, identifying this as progress.
Objective Content
This section needs to at a minimum include 3 statements/shares/concepts discussed by the client during the session along with at minimum 3 statements about the therapeutic interventions the therapist used with the client during the session. Please be aware that the 3 and 3 rule is a minimum and it is expected that your note be more detailed with explanations and reasons for the interventions and including details about what the client shared during the session (quotes from the client are a great way to add additional information into your note). This should be a comprehensive summary of the entire session (see examples below). This should also include how the interventions are helping the client reach their therapeutic goals/objectives and be closely related to the goals set up for treatment.
- For notes that are 45 minutes (90834) and 30 minutes (90832) long - a 2 and 2 rule may be used
- For a 30 minute note that had a duration of 16 minutes - a 1 and 1 rule may be used (anything above 16 minutes needs to follow the 2 and 2 rule)
Examples
- When the client disclosed her husband’s intentions of opening a taproom, the clinician offered exploration of emotions in order to model for her the importance of giving voice to her opinions. The client stated that she is ambivalent about it and has been trying to manage her expectations because her husband has had dreams that have not come to fruition before and she does not want to get disappointed. She also reported that she worries and that her thoughts are “here we go again: he will be super busy and will never be home.“ The clinician offered a cognitive challenge by asking the client if she has shared these concerns with her husband and when the client denied the clinician encouraged her to identify and verbalize potential benefits and costs of doing so. The client stated that the only cost is the effort of speaking up when she is “used to keeping things to myself and always acquiesce to my husband, which leads me to harbor negative feelings”. She was able to identify benefits such as “easing my mind, learning how to become more assertive and respect myself, and setting a boundary with my husband.“ Discussion ensued on assertive communication and the client role-played with the clinician in order to increase her level of comfort in her ability to share her views with her husband.
- The main themes of the session were:
Client reported distressing communication with her intimate partner and the end of their relationship, including an abusive email and phone call from her partner, in which she reported he called her a "manipulative, lying, awful person." Clinician provided supportive reflection, and psycho-education in order to aid the client in deepening her understanding of her emotions, specifically feelings of hurt and abandonment. Client discussed concerns about her role in the intimate relationship and how to navigate mutual friendships. Clinician provided cognitive challenging, and reframing to assist the client in recognizing how her thinking patterns are affecting her relationships in a negative way and how she can change thoughts such as “I’m a bad person” into “I like myself and I deserve happiness.” Clinician utilized solution-focused therapy to guide the client to identify potential challenges this week and identify strengths and coping skills to utilize to help her get through difficult emotions this week. One specific coping skill the client will focus on that was discussed during the session is using radical acceptance. Clinician provided exploration of coping patterns to guide the client in developing healthier ways of managing challenges in the future. The client agreed to try to implement at least 3 skills provided in the upcoming week.
- The clinician helped the client explore emotions related to feeling like she's "not doing enough" and doesn't deserve what she's worked for. The clinician helped the client identify relationship patterns that have contributed to her feeling this way in her life. The clinician helped the client identify why they revert to some of their negative or unhealthy coping patterns based on past behavior and coping strategies they employed in their childhood. The clinician helped the client challenge distorted beliefs and thinking patterns, especially related to self-worth, and reframe them to be more accurate and supportive thinking patterns. The clinician used EMDR and IFS to help the client process past traumas and negative experiences related to their birth mother's treatment of her. The clinician used supportive reflection to empathize with the client and encourage them in how hard they've worked and how much they've overcome. The clinician used psychoeducation to help teach the client about ego states and how we can slip into and act from past ego states that can affect how we respond to situations and our ability to make appropriate and desirable decisions that we would make if we were acting from our healthy adult state. The clinician helped the client learn ways to notice their negative thoughts and taught them the importance of replacing those thoughts with more accurate and supportive ones from our 'adult' self. The clinician used interactive feedback to reflect back on what the client was reporting with appropriate insight and responses.
Interventions Used
Check only the boxes of the interventions used during this session. In the Other: box you can add any additional interventions you used that are not listed. For example: Cognitive Behavioral Therapy, EMDR, Synergetic Play Therapy, Validation, Art Therapy, Gottman Couples Counseling, etc.
Example
Communication Skills, Compliance Issues, Exploration of Coping Patterns, Exploration of Emotions, Exploration of Relationship Patterns, Interactive Feedback, Interpersonal Resolutions, Structured Problem Solving, and Supportive Reflection
Treatment Plan Progress
Objectives will automatically be populated from the TP. For the Progress: box - click in the box and choose from the options given such as Improved, Maintained, Progressing, Regressed, etc. You can alway write your own description here such as Slight Progress, or Mild Regression, etc.
- You can also add an additional comment after the choice you make to explain how the client is demonstrating their progress or regression.
Example
1.2) Client will practice utilizing various grounding techniques 4 times per week as evidenced by self-report.
Progress: Progressing as evidenced by the client using journaling and listening to music to alleviate herself from anxiety symptoms.
Additional Notes / Assessment
Here the clinician can write additional comments about the client’s progress toward reaching their goals/objectives. Therapists can also document the teletherapy session, location of the client, and ability to speak confidentially in this section.
Examples
- Overall progress since starting treatment has been high as evidenced by the client's ability to quickly establish trust and rapport with the therapist in order to share her negatively impacting relationship with her mother and practice self-regulation skills. The therapist realized she needed to add a coordination of care goal to the treatment plan and will be subsequently adding one prior to the next session.
- Client reported she plans to utilize self-care and coping skills she's learned in therapy to get through this week. Client reported she is feeling "more like myself than I have in a long time." Clinician observes client demonstrates progress by recognizing and taking responsibility for working through her emotions, evidenced by client report of emotions and use of coping skills. Client's prognosis is excellent because of her willingness to engage in therapy sessions, strong therapeutic rapport, and openness to utilizing techniques to improve her symptoms outside of sessions.
- Possible relevant information:
- If the client was given multiple diagnoses in the intake session and one (or more) of the diagnoses are not being treated and have been documented in the intake note and the TP an explanation of why that diagnosis is on the progress note and not discussed would go here:
- As an example - MDD and Alcohol Use Disorder were both given and the current treatment is currently only focused on MDD a statement similar to the following will be included here:
- The client continues to receive outside care for the SUD diagnosis through AA.
Plan
Here the therapist will write what the plan is for the next session. This may include homework assignments, time and date of next session, type of session (individual, couples, etc) topic for discussion in the next session, etc.
Tip: It is recommended to include information about what will be done in the next session, whats expected to occur between sessions, etc.
Examples
- The date and time of the next session will be Friday, June 25th, 2021 at 11am. The session will be an individual session between the client and this therapist. The plan for the next session will be to continue processing emotions around this traumatic experience Client will continue to attend weekly individual therapy sessions on Tuesdays at 2pm to process feelings and manage stress while building coping skills to reduce symptoms of adjustment disorder. Clinician will continue to provide cognitive-behavioral techniques and coping skills while working on some of the underlying causes of her anxiety. Clinician will focus on providing self-regulation techniques for client in preparation for trauma healing related to client's triggers.
Prescribed frequency of treatment
The clinician chooses how often the client will be engaging in treatment - weekly, monthly, etc.
Recommendation
The clinician chooses what the recommendation for treatment is: Continue current therapeutic focus, Change treatment goals or objectives, or Terminate treatment.
How to get the TP to populate into a progress note when updating a TP during that session (same day)
- At the 150 day mark when a TP needs to be reviewed at least part of a session must be devoted to treatment planning until it is complete and this needs to be documented in the progress note.
- An Auditor should see both a new TP and a progress note describing the treatment planning process.
Interventions
Interventions used with clients
You do not have to only use the interventions TherapyNotes gives you in the interventions Used section which are:
Cognitive Challenging, Cognitive Refocusing, Cognitive Reframing, Communication Skills, Compliance Issues, DBT, EMDR, Exploration of Coping Patterns, Exploration of Emotions, Exploration of Relationship Patterns, Guided Imagery, Interactive Feedback, Interpersonal Resolutions, Mindfulness Training, Motivational Interviewing, Preventative Services, Psycho-Education, Relaxation/Deep Breathing, Review of Treatment Plan/Progress, Role-Play/Behavioral Rehearsal, Structured Problem Solving, Supportive Reflection, and Symptom Management.
You can add any additional interventions you use with clients into the “Other” box.
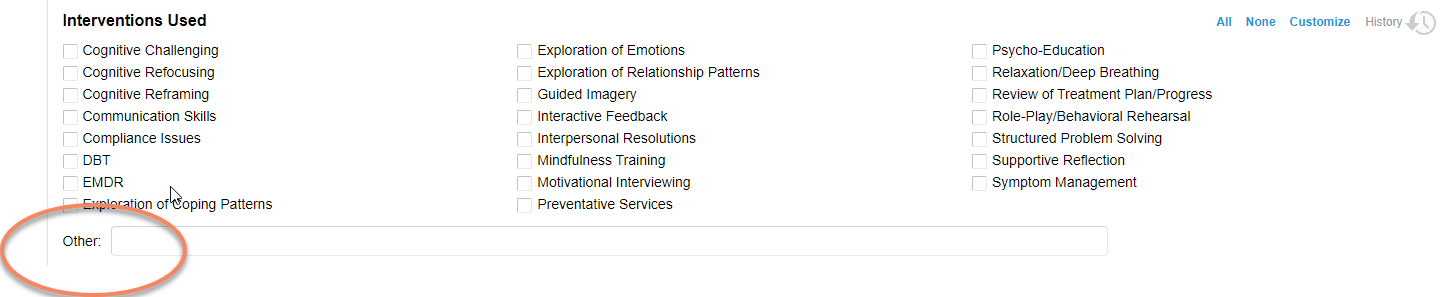
Here are some examples of other interventions you may be using with clients during your sessions:
- Miracle question
- Open-ended questions
- Appropriate use of silence
- Paraphrasing
- Reflection, Reflecting back
- Summarizing
- Acknowledgment
- Empty chair
- Focusing on repressed emotions
- Exploration of decision making
- Building self-efficacy
- Enhancing self confidence
- Positive visualization
- Taking an inventory
- Exploration of triggers, identifying triggers
- Modeling acceptance
- Transforming troublesome thought patterns
- Deconstruct harmful thought patterns
- Breaking negative connections
- Journaling to track behaviors/thoughts/actions,etc
- Encouraging a more positive mindset
- Meditation
- Reinforcement
- Operant conditioning
- Identifying maladaptive beliefs
- Processing traumatic memories
- Gradual exposure
- Taught behavior management techniques
- Teaching self-regulatory skills
- Paradoxal Interventions
- Behavior Reinforcement
- Anger management
- Collaborative Problem-Solving
- Labeling feelings
- Stress management
- Empty chair
You may be doing the following types of therapy with clients that can be added to the “Other” box as well:
- Dance/Movement Therapy
- Play Therapy
- Art Therapy
- Laughter Therapy
- Drama Therapy
- Music Therapy
- Positive Psychology
- Brain Spotting
- EFT
- Gottman Couples Counseling Techniques
- Sandplay
Descriptive Intervention Words
- Asked
- Assisted client in
- Acknowledged
- Affirmed
- Challenged
- Clarified
- Coached
- Collaborated
- De-escalated
- Demonstrated
- Developed
- Directed
- Discussed
- Encouraged
- Explained
- Examined
- Explored
- Evaluated
- Facilitated
- Focused on
- Gave homework
- Guided
- Instructed
- Interpreted
- Introduced
- Inquired about
- Listened
- Paraphrased
- Performed
- Planned
- Practiced
- Praised
- Prompted
- Provided
- Redirected
- Reflected back
- Reframed
- Refocused
- Reinforced
- Responded to
- Reviewed
- Role played
- Set boundaries
- Shared
- Supported
- Trained
- Validated
Sample Wording
- The therapist used supportive reflections and interactive feedback to draw out what the client and therapist have discussed in past sessions regarding the client's difficulty to express her emotions and set boundaries due to excessive feelings of fear and guilt.
- Clinician engaged the client in a solution-focused approach in order to assist the client with increasing self-care and self-awareness to help with the stress and overwhelm from home and school.
- Clinician provided compassionate inquiry, supportive reflection, and exploration of emotions to deepen client’s insight into the experience and facilitate the processing of feelings.
- The clinician encouraged relaxation and deep breathing to help aid the client in healthy coping patterns and containment.
- The clinician used MI OARS skills to assist the client in identifying early warning signs (i.e., "it feels like a wave" (of stress)) and triggers (i.e., increased heat, mom) for her psychogenic triggers.
- The therapist used DBT to introduce Radical Acceptance to the client and explored with the client what Radical Acceptance looks like with her children in the present.
- The clinician assisted the client by providing interactive feedback and supportive reflection to validate the client’s feelings and experience.
- The clinician discussed with the client developing a thought journal to track negative thoughts throughout the week and using if-then statements to better identify these negative beliefs.
- The clinician asked open-ended questions to the client to allow her time to process happenings during the week.
- Therapist normalized the difficulty of this process and highlighted her growth in it and engaged her in identifying and processing underlying fears to opening up with her husband.
- Positive parenting techniques were discussed and client practiced directions, praise, and ignoring skills in role-play exercises.
- The client and therapist discussed some of the client's interests and goals for therapy as part of rapport building.
- This clinician guides the client through guided imagery of a stream and assists him in using mindfulness to create the scene in his mind.
- Clinician acknowledged statements, and gently challenged client to elaborate, "what do you mean by that?"
- Clinician utilized solution-focused therapy, and structured problem-solving to guide the client to identify opportunities to build on her growth and continue to make positive decisions that move her forward toward her goals.
- Clinician provided communication skills and behavioral rehearsal to guide client to practice recognizing and verbalizing her needs.
- The clinician used MI skills including open-ended questions, reflective listening, affirmation, and summarization to assist the client in identifying and creating her treatment plan goals.
- Clinician had the client participate in a role-play and demonstrated how to ask clarifying questions that can prevent misunderstandings and fights in the future.
- The therapist and client reviewed the DBT information that the client received at her last appointment and the client will reread the information this week about distracting from self-destructive behaviors.
- The therapist used interactive feedback, and cognitive challenging to explore the impact that not addressing this issue directly with her friend is having on her self-esteem and coping strategies.
- Therapist engaged her in identifying the unhelpful thought and the root of fear and how she sees herself in relation to God as well as how this thought reflects the way she thinks about God's character and she was able to process underlying thoughts, beliefs and emotions with therapist and able to reframe this thought into a more helpful thought.
- The clinician validated the effort the they both made in following through with the homework and the results that they have seen in one week.
- The therapist affirmed the client's empowerment, as the client has had much difficulty saying no in the past.
- The clinician used if-then statements with the client during the session to identify and challenge her belief that she's unlikeable to others in her field.
- The clinician used Socratic questioning when helping the client identify and challenge her negative beliefs "I'm not worthy" and "I'm always wrong."
- Clinician utilized solution-focused therapy and strengths-based perspective to guide client to identify how she can utilize this new insight to change the way she approaches difficult situations.
- The clinician provided identification and practice of several visualization meditations to the client to offer coping tools to start managing her anxiety in between sessions.
- Clinician engaged the client in a CBT exercise to explore what the client can control and what she can't in order to assist the client in increasing her executive functioning skills.
- This clinician provides psycho-education on coping skills to decrease emotional intensity immediately after a triggering event.
- The clinician used open-ended questions, reflective listening, and summarization when exploring how the client's family values and religion influences feelings of guilt and worked with the client on reframing her perspective on "gossip" (i.e., not gossip if sharing her story to others).
- Clinician provided exploration of coping patterns to guide client to identify and recognize her tools and ability to cope with her distress.
- The therapist provided psycho-education regarding a weekly State of the Union meeting in which she and her husband have a safe, neutral, and structured space/time to share the good and difficult things in their relationship, as well as the Family Logistics Meeting in which the client and her husband can discuss their weekly plans and include discussing self-care in the plans.
- Therapist again encouraged her to communicate clearly her expectations and boundaries within her personal and work life to feel comfortable and safe in every way and she noted understanding and agreement.
- Clinician provided mindfulness training, DBT, and relaxation/deep breathing in guiding client to practice grounding techniques for regulating emotions.
- The clinician taught the clients about using Mindfulness to avoid worry about their future together which can lead to worry, fear, and doubt about their marriage.
- The clinician provided the client with psychoeducation related to the importance of clear and consistent boundaries.
- The therapist used cognitive reframing to remind the client that she also deserves to have her feelings and experiences considered within her relationships.
- The therapist introduced the control/responsibility matrix and the client and therapist identified what the client is responsible for and in control of (what she says) and what she is not (how her brother responds and what he does).
Progress Note for Couples
For the progress note documentation will be written according to normal standards for progress notes with a focus on the “client” the couple/family. For example:
Risk Assessment
Patient denies all areas of risk. No contrary clinical indications present.
Medications
Client and spouse did not report changes in medications. Client and spouse both previously reported they take no medications.
Symptom Description and Subjective Report
This session was conducted via telehealth. Client and spouse reported they were in the privacy of their own home and able to talk freely. Client arrived to the session 5 minutes late with an unremarkable presentation, apologizing for being late due to computer trouble and displaying appropriate distress while discussing distressing topics. Client reported feeling "disconnected" from spouse and feeling like she is "bothering him" with "things that shouldn't be bothering him." Client also reports feelings of anxiety, worry, and distress about “if the marriage can last.” Client's spouse reported he has been feeling stressed and irritable and has had difficulty sleeping which has made him feel disconnected. Client and spouse displayed distress through tears and verbal statements of pain, shame, and "abandonment" while discussing childhood trauma in this session. The clent reports the distress has occurred 5 out of 7 days of the past week, the distress lasted for “at a minimum three hours” for each event. The severity of the client’s symptoms is moderate based on the impact it is having on the couples ability to engae fully in their daily jobs as well as the impairment they are feeling in their own relationship to communicate effectively with one another.
Objective Content
The main themes of the session were:
Client and spouse discussed stress since their last session, including positive stress of moving forward in their careers and negative distress of the anniversary of their dog's death on Sept 2. Client and spouse discussed how individual therapy has helped and has been stressful lately with insurance difficulties. This clinician provided exploration of emotions, supportive reflection, exploration of coping skills, somatic experiencing and emotion-focused therapy to deepen client and spouse's awareness of their experience and facilitate processing and connection together.
This clinician facilitated a conversation about how sadness was expressed in their homes in childhood. This clinician provided exploration of emotions and emotion-focused therapy to facilitate connection between them and normalize their difficulty in processing this emotion. This clinician provided solution-focused therapy, strengths-based perspective and cognitive refocusing to guide client and spouse to identify how they have overcome some of these barriers.
Client and spouse both discussed distress regarding the trauma of their fathers not being involved in their lives. This clinician provided emotion-focused therapy, exploration of emotions and supportive reflection to deepen client and spouse's awareness of their and each other's emotional experience and facilitate connection between them.
This clinician led the client and spouse through somatic experiencing exercise to release some of the traumatic distress and self-regulate to move forward with the day. Client and spouse both reported feeling a sense of calm after the exercise. This clinician provided psycho-education and relaxation/deep breathing to aid in this process.
This clinician facilitated conversation for client and spouse each to identify one way they can support each other during this time-- client named asking how her day is, spouse named spending time together doing something enjoyable like watching funny tv shows.
Reasons for Rejected Notes
In progress notes, not giving at least 3 things discussed by the client during the session as well as at least 3 therapeutic tools/interventions you used with the client during the session.
Planners
Find helpful notes samples/guides/text on our Google Drive: Shared Drive >> Therapy Resources >> Psychotherapy Planners.