Intake Note Expectations
Counselors, follow the instructions below on how to write an Intake Note. Remember, notes need to be written within 72 hours of DOS. Read more here: Note Writing Timeliness Policy. Are you tired of writing notes? Use our AI Scribe.
Good Intake Note Example(s)
How to write an Intake Note video
Intake Note Slideshow
Make sure you are always using complete sentences, correct grammar, and correct spelling. This is a professional document, and it needs to be written as such. You can use the spell check button at the bottom of the note and download Grammarly to your computer to help you catch grammatical errors.
Note Header
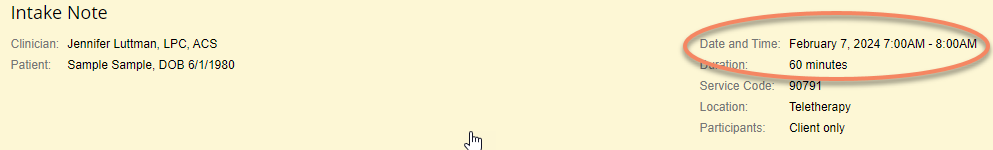
The below image is a sample Intake Note Header unchanged by the clinician (auto-populated by TN): (90791, 60 minutes, 7:00 am - 8:00 am)
Insurance wants to see the actual Face-to-Face time put in this note header not the auto-populated information. In the note header, click on the “Edit” button and adjust the time that appears in the white box.
The below image is a sample Intake Note Header that the clinician has changed to reflect the actual face-to-face time they spent with the client: (90791, 55 minutes, 7:04am - 7:59am)
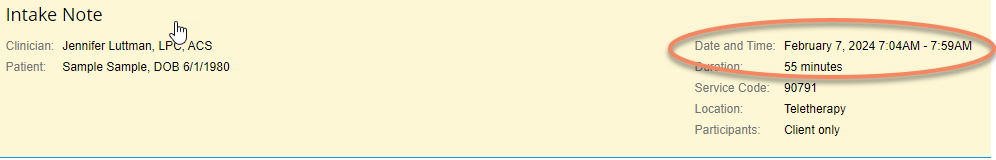
The time could start early, start on time, start late, end early, end on time, or end late - any of these are allowable and are what insurance wants to see as far as the “Duration” of the session goes.
Presenting Problem
- major symptoms (what brought the client to treatment)
- how symptoms have progressed
- situations in which it is worse or better
- what has been tried to improve symptoms
- what worked in the past if this is a recurrence
Presenting problem section - These can not be vague. You can include quotes from the client about the reasons they are coming in for treatment. This is where you begin to set the stage for what the diagnosis is going to be for the client.
Here are a couple of examples of a great presenting problem:
- Client reported she is seeking help through therapy to overcome feelings of sadness and depression and "get back to glowing." Client reported poor appetite, worry about the future, difficulty sleeping, racing thoughts, low mood, fatigue, regret, self-blame, and low self-esteem. The client reports these symptoms are most obvious in her work environment as she has been “calling off from work at least once a week,” and she is afraid of getting fired. The client has attempted her own self-help techniques, but reports that they have been unsuccessful in decreasing her symptoms.
- The client reported having emotional or behavioral symptoms marked by ongoing feelings of sadness, despair, loss of energy, and difficulty dealing with normal daily life. The client reported she has been experiencing more stress and anxiety starting at the end of last year, and she stated it has increased by "at least 50%." The reports she has lost relationships in her life, and feels like she is not being the mother she knows she could be to her children. She reported she has been diagnosed with depression in the past and sought out therapy, which was “mildly helpful” but only lasted for 2 months due to the client moving. The client stated she would like to learn better ways to cope with her stress and anxiety, which is why she sought out therapy as her own attempts to decrease her symptoms have “not helped.”
Current Mental Status
You can check “all normal” and then modify according to what the client presents in the session.
Example: For a depressed client, you would want to change their mood from Euthymic to Depressed, or change their Affect from Congruent to Flat, etc.
Risk Assessment
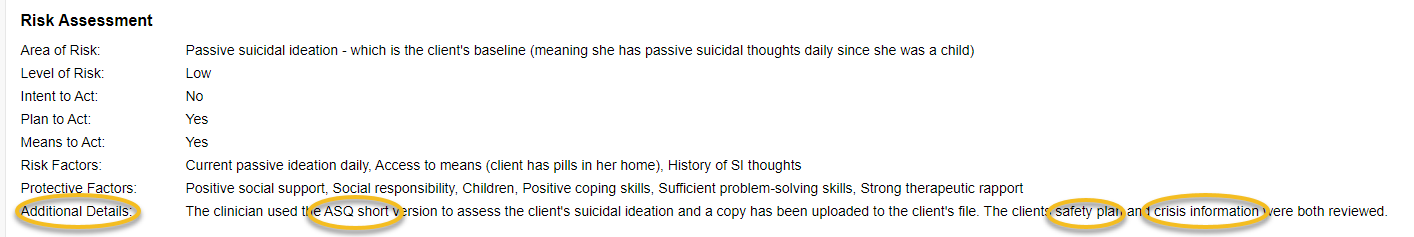
Check the box - Client denies all areas of risk. No contrary clinical indications present - if the client reports no risks. If the client is reporting risks (within the past 30 days to present), then include the area of risk, the level of risk, intent to act, plan to act, means to act, risk factors, and protective factors.
3 required steps:
- Conduct a risk assessment - ASQ or Columbia. The risk assessment must be uploaded to the TN file (and documented in the additional details box)
- If the client has a positive screen for SI or HI, you must create a safety plan (and document it in the additional details box). If the client has been hospitalized in the last 90 days, a safety plan must also be written.
- The safety plan must be uploaded to the TN file and must be signed by the client.
- This can be sent via the portal for e-signing or signed in person and uploaded.
- In addition, we must review emergency/crisis information with the client (and document this review in the additional details box)
Example from TN:
Objective Content
2 mandatory items - reviewed the disclosure statement and coordination of care - see below.
Include here what you did during the intake session to include the documents that were discussed by the clinician such as: HIPAA, No show policy, Disclosure Statement, Mandatory reporting, Medicaid 3 strike policy (only if a Medicaid client), confidentiality, etc. ROI if necessary.
Example
Clinician asked if client had any questions about the paperwork the client had signed prior to the session; client reported having no questions. Clinician reviewed the disclosure statement, confidentiality, mandatory reporting guidelines, cancellation policy, no show fees, Medicaid 3 strike policy, client reported no questions or concerns. The therapy session was conducted between the therapist and the client using therapyportal video chat software. The client reported their location was in their home and they reported sufficient privacy to conduct a teletherapy session. The clinician asked the client about speaking with either her primary care physician (PCP) or other mental health providers. The client declined coordination of care for now. The client is engaging in couples counseling so an ROI will be signed for the client’s spouse to participate in treatment.
If you are working with a client who is 12-15 you must also document the following per the Revised Statutes, Mental Health Section 12-245-203.5.
- The mental health professional shall engage the minor in a discussion about the importance of involving and notifying the minor's parent or legal guardian and shall encourage such notification to help support the minor's care and treatment. See example documentation below.
- Notwithstanding the provisions of subsection (3)(a) of this section, a mental health professional may notify the minor's parent or legal guardian of the psychotherapy services given or needed, without the minor's consent, if, in the professional opinion of the mental health professional, the minor is unable to manage the minor's care or treatment.
- A mental health professional described in subsection (1) of this section shall fully document when the mental health professional attempts to contact or notify the minor's parent or legal guardian, and whether the attempt was successful or unsuccessful, or the reason why, in the mental health professional's opinion, it would be inappropriate to contact or notify the minor's parent or legal guardian. Documentation must be included in the minor's clinical record, along with a written statement signed by the minor indicating that the minor is voluntarily seeking psychotherapy services. This would be documented as a contact note in the client’s file.
Example
The clinician discussed the importance of involving parents/guardians in the minor's treatment. The clinician encouraged the client to sign an ROI, allowing the clinician to speak with parents/guardians. The client (either agreed and an ROI has been uploaded to their file, or declined, so no ROI will be signed).
Teletherapy sessions
If the session was a teletherapy session, you must include a statement about the client’s location and their ability to speak freely/confidentially during the session. For example:
Examples of how you can write the statement about it being teletherapy:
- This session was conducted via teletherapy.
- The session was held via teletherapy per the client's request.
- The therapy session was conducted between the therapist and the client using Client Portal video chat software.
Examples of how you can write the statement about the client's location (specific address is not required):
- The client confirmed that she was located in her mother's office, and she confirmed that she had privacy and could talk freely.
- The client reported their location was in their home, and they reported sufficient privacy to conduct a teletherapy session.
PCP Preference
During an intake, we need to ask if the client has a PCP or other health care provider that they would like us to be in contact with. In the intake note in the objective content section, we need to include a statement about asking the client about this and if they agreed or declined. Here is an example of how that could be worded (but feel free to use your own wording): "The clinician asked the client about speaking with either her primary care physician (PCP) or other mental health providers. The client declined this contact for coordination of care for now." Or: "The clinician asked the client about speaking with either her primary care physician (PCP) or other mental health providers. The client stated she would like the clinician to contact her Psychiatrist, so an ROI was filled out and will be uploaded to the portal.”
If they say yes, then we need them to fill out an ROI and get it uploaded into their TN account, and then reach out to the provider and document that we have made a contact attempt or were able to speak with the provider.
Also, then go into the client's file in the patient info tab, edit, click on the dropdown menu for PCP Release, and choose the appropriate option if the client declined or agreed.
Here is how to do that:
- Click on the Patient Info tab
- Click edit in the patient information box (you can click anywhere in the box)
- Click in the drop-down box labeled "PCP Release."
- Choose the appropriate option per the client's choice:
- Patient consented to release information: (an ROI must then be sent/given to the client to fill out). Once the ROI has been filled out and uploaded, the therapist needs to make contact with the person listed and add a contact note in the client’s file that you have attempted to contact the person or did contact the person.
- Patient declined to release information: Not applicable (this should only be used if the client does not have a PCP or other mental health provider, and this must be documented in the intake note).
5. Scroll to the bottom - click on Save Changes
Here is a picture of where this is located in TN:

**Every client needs to have this box appropriately filled in; it can not be left undone.
ROI
If anyone else is (or will be) attending the session or the therapist will be speaking to them about anything to do with treatment the client needs to fill out an ROI with that person’s name so the clinician can speak with them. This includes all couples and family sessions.
Work Hours
Speak with your clients about your availability/work hours so that they understand the guidelines around when they can expect to hear back from you. Remind clients that you are not a crisis provider and that they have other options if they enter into a crisis situation.
Review the "Availability and Response Policy" found in our disclosure statement with the client. Be sure to document this communication in the note.
Biopsychosocial Assessment
Include as much information as you can gather from the client during the session, and also look over their intake questionnaire to aid you in filling in the boxes. Each question needs to be filled in with a remark. If the client denies or states they have nothing to report about that question, you can state “None reported by the client” or “Client denies,” but never leave a box empty.
Identification: (age, ethnicity, religion, marital status, referral status, etc)
Client reported she identifies as a 30-year-old Asian female, wife, and mother with no religious or cultural affiliation.
History of Present Problem: (symptoms, onset, duration, frequency, etc)
This is where medical necessity is demonstrated for the diagnosis (or diagnoses).
- Symptom onset
- Symptoms
- Frequency of symptoms
- Duration of symptoms
- Severity of symptoms (mild, moderate, severe) (Likert scale)
- Impairment/impact on functioning
If the client has been given multiple diagnoses, then the above 6 medical necessity pieces of information must be provided for each diagnosis.
This is not a copy of the presenting problem.
The client reported that symptoms of major depressive disorder began in roughly January of 2021 due to multiple moves, a divorce from a toxic relationship, and separation from her child. The client reports that she did not experience any symptoms of depression prior to January 2021. The client's symptoms of major depression include: low mood, anhedonia, sleep/appetite disturbances, fatigue, feeling bad about herself, difficulty concentrating, psychomotor retardation, and SI. The client reported these symptoms have occurred daily for at a minimum of 3 hours each day, all the way to all 12 hours of her day. The client reports depending on the day, the severity of these symptoms is moderate-severe and they impact her ability to get out of bed, be a good mother, engage in getting a new job, and maintain strong relationships with others.
Psychiatric History: (prior episodes of symptoms, diagnoses, courses of treatment, etc.)
Client reported she struggled with depression, anxiety, and low self-esteem throughout most of her life, but has felt it was manageable. Client reported she has done counseling a few times over the years and has sometimes found it to be helpful. Client reported she attended marriage counseling with her spouse for 2 years 3-4 years ago and found it to be helpful for their relationship and communication. Client reported she and her spouse are currently attending weekly couples therapy sessions. (Can not be vague - if the client has a psychiatric history, include as much information as possible: dates, duration, what for, etc).
Trauma History: (nature of trauma, when it occurred, persons involved, etc.)
Client reported she found out her boyfriend in college was cheating on her the day before she was scheduled to take the LSAT for law school, and bombed the test the following day. Client reported she has no other traumatic experiences in her history. (Can not be vague - if the client reports a trauma, include as much information as possible: dates, what occurred, symptoms occurring after the trauma, results of the trauma (court, divorce, etc), or add a statement that the client refused to discuss the trauma further at this time.
If the client reports child abuse (even if they are over 18), a statement must be made about whether the abuse was reported previously, if not, will it be reported now, and if it will not be reported now, why not?
Examples:
- The abuse of the minor has never been reported; therefore, this clinician called the Child Abuse Reporting Hotline (1-844-264-5437) on (date) at (time). This clinician spoke with (name of person you spoke with), and the case number is (#).
- (Client over 18) The alleged perpetrator of the abuse is deceased; therefore, no report will be made.
- (Client over 18) The alleged perpetrator of the abuse is not in a position of trust and does not have access to minors; therefore, no report will be made at this time. If additional information is provided in the future that requires a report, it will be made at that time.
Family Psychiatric History: (history of mental illness in family, diagnoses, etc.)
The client reported on her intake paperwork that her mother and sister have been previously hospitalized for mental health concerns, but did not provide additional information.
Medical Conditions & History: (current and past medical conditions, treatments, allergies, etc.)
Client reported she has irritable bowel syndrome, which she takes medication for, and that has not changed recently. Client reported no other medical conditions.
Current Medications: (medication, dosage, purpose, prescribing physician)
Client reported she is currently taking the following medications prescribed by her PCP: duloxetine 30 mg once daily for anxiety (which she reported she has been taking consistently for 2 years and feels it helps her) and Colestipol for irritable bowel syndrome. The client did not know the name of her PCP.
Substance Use: (history of substances used, including alcohol, tobacco, and prescription drugs other than as prescribed, etc.)
Client reported she drinks from one glass of wine to ½ bottle of wine each night with dinner. Client reported she drinks about 1/2 cup of coffee each morning for caffeine. (Include family history of substance use - If none exists - “The client denies any family history of SUD issues.
Family History: (family of origin, relationship with parents, siblings, significant others, etc.)
Client reported she grew up in Boulder in a "normal" life where her dad worked for the government and her mom was a secretary. Client reported she had no siblings, and her parents are still married. The client was previously married for a year when she was 20 and went through a divorce of that marriage. Client currently lives with her husband, their 3 children, and their cats.
Social History: (significant relationships, social support, nature/quality of relationships, current community resources, etc.)
Client reported "making friends has always been a challenge" because of her low self-esteem, naming herself as "introverted" and "socially awkward." Client reported she does have several friends who know what she is going through and who she talks to regularly, mostly through texting.
Spiritual/Cultural Factors: (important spiritual practices and communities, cultural influences, etc.)
The client denied any spiritual affiliation and identifies as Caucasian. She denied any concerns that her religious or cultural affiliation would have an impact on her treatment.
Or -
The client does not identify as spiritual; however, they do identify as cultural. The client's cultural background and factors will be integrated throughout treatment through cultural sensitivity and using a multicultural therapeutic approach.
Include a statement about whether this (spiritual/cultural factor) will have an impact on treatment or not.
Developmental History: (developmental milestones, delays, etc.)
The client did not disclose any significant developmental history, but states, "I think I did everything on time."
Educational/Vocational History: (level of education, current/past employment, hobbies, leisure activities, etc.)
Client attended CU Pueblo for her Bachelor's and Master's degrees and is now a teacher. The client enjoys hiking, bike riding, and “doing pretty much anything outdoors.”
Legal History: (arrest/summons history, sentencing, DUI occurrences, incarceration, civil litigation, family court matters, etc.)
The client denied any significant legal history other than her involvement in the courts for her prior divorce.
SNAP: (strengths, needs, abilities, preferences, etc.)
S: The client reports her strengths are that she is loving, kind-hearted, and sincere.
N: The client reports her needs are to process her trauma, develop coping skills, and increase her mindfulness skills. The clinician identifies her need to create a safety plan for her current SI.
A: The client reports that her abilities are that she has average intelligence, she is able to read/write, she has computer skills that allow her to access teletherapy sessions, she has transportation so she can attend in-person sessions, and she reports that she has good insight into where her trauma comes from, which will aid her in the therapeutic process.
P: The client reports her preferences are to have in-person sessions as much as possible, meet with a female therapist, and have sessions in the evenings after work.
Other Important Information: (other important information relevant to treatment)
The client was given the PHQ-9 and received a score of 25/27, indicating severe depression.
TN says this section is for “other important information relevant to treatment.”
Possible relevant information:
- Including an explanation if the client was given multiple diagnoses and one (or more) of the diagnoses is not going to be included in the treatment between the clinician and the client
- As an example - MDD and Alcohol Use Disorder were both given and the treatment will solely be focused on MDD a statement similar to the following will be included here:
- The clinician has recommended the client seek treatment for their Alcohol Use Disorder through referrals given to them for outside providers that treat SUD diagnoses and engagement in programs such as AA and Smart Recovery.
- As an example - MDD and Alcohol Use Disorder were both given and the treatment will solely be focused on MDD a statement similar to the following will be included here:
Plan
Include what the plan is moving forward with the client. What will future sessions look like?
Plan Section - In this section, we need to be sure to include the following three items:
- Initial goals for treatment (you can also include your proposed interventions before the treatment plan is developed).
- Recommended type and frequency of services.
- Whether referrals are needed for additional services.
Here are some examples of how this could be worded:
- The client expressed the following goals for treatment: "to understand how to heal from this, the worst trauma I have ever experienced," and "to feel more confident in my decisions" in deciding how to move forward with her life. The client will attend weekly individual therapy sessions where the clinician will offer coping, grounding, and self-regulation skills and provide support and guidance in processing the client's distress. No outside referrals are appropriate at this time.
- The initial discussed goals for treatment are for the client to reduce symptoms of other specified depressive disorder and for the client to report her overall wellbeing as 9 out of 10, with 10 being the highest. See the treatment plan document for the full treatment plan. Treatment is recommended as individual weekly sessions. No referrals are needed at this time; however, if the need arises, the clinician will make the appropriate referrals to outside agencies.
Diagnosis
You must use an F code as the primary diagnosis code. You may use a Z code as a secondary diagnosis, but not as a primary diagnosis. Underneath the diagnosis, you must include the symptoms the client reported that meet the diagnostic criteria for the diagnosis you have given the client. Use the DSM language in order to demonstrate that the client meets the full criteria for the diagnosis given (ie - each of the criteria, A,B,C,D,E, etc).
Diagnosis - under the diagnosis given to the client, it must also be "person-specific information" about how the client meets the criteria for the diagnosis. Here are some examples of how to word this:
F430 Adjustment Disorder, Unspecified
Z630 Relationship Distress with Spouse or Intimate Partner
The client reported symptoms of adjustment disorder, unspecified in the form of distress related to the relationship (lack of trust, hurt feelings, anger) and communication issues (yelling, storming out on one another, shutting down). The client reported this distress developed in response to and less than 3 months after the client learned about her husband’s affair and has persisted for fewer than 6 months after onset. The clinician evaluates the stressor as causing significant distress and impairment in social and occupational functioning for the client. The clinician evaluates symptoms as not representing normal bereavement. Client does not meet criteria for another disorder at this time.
F430 Post-Traumatic Stress Disorder, Unspecified
The client reported the following symptoms that meet the diagnostic criteria for PTSD: She has directly experienced a traumatic event. She has recurrent, involuntary, and intrusive distressing memories of the traumatic event, which occur daily. She is having recurrent distressing dreams in which she is reliving the traumatic event, and she can’t escape. The client expressed intense or prolonged psychological distress (hyperventilating, feeling like she needs to flee, heart racing, intense fear) at exposure to driving a vehicle or seeing a car accident that resembled her traumatic event. The client reports she avoids external reminders (people, places, driving, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about her traumatic event. The client reports an inability to remember important aspects of the trauma, by stating “it’s like certain memories are kept from me,” and she experiences a persistent negative emotional state of fear, which she says is present daily. She reports irritable behavior toward friends and family and angry outbursts that come out of nowhere, and an exaggerated startle response, specifically when in or near cars. The duration of the disturbance is more than 1 month. The disturbance causes clinically significant distress in social and occupational areas of her functioning. The disturbance is not attributable to the physiological effects of a substance.
F41.1 Generalized Anxiety Disorder
The client reported the following symptoms that meet the diagnostic criteria for generalized anxiety disorder: She experiences excessive anxiety and worry about her previous and current relationships, her ability to obtain a job, and her future living situation, occurring nearly every day for the past two years, and finds it difficult to control the worry (ruminative thoughts). She reported her anxiety manifests in the form of feelings of restlessness (difficulty relaxing, increased heart rate), being easily fatigued (physically and mentally), difficulty concentrating (indecisiveness due to overthinking), irritability (toward herself and others), muscle tension (per her report), and sleep disturbances (difficulty falling/unsatisfying sleep). Her symptoms are not attributable to the effects of substance use, another medical condition, or another mental disorder.
DSM-5 Diagnosis Tool
You can add multiple diagnosis codes here:
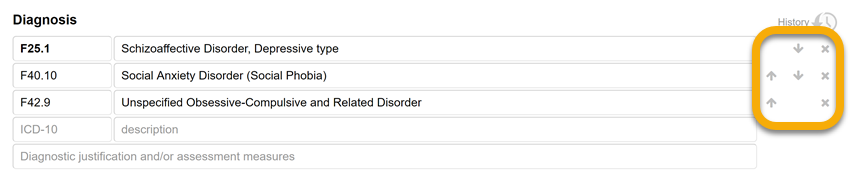
The first diagnosis code in your list, which appears in bold, is the primary diagnosis and will be used for billing. Electronic (EDI) claims may include only the primary diagnosis code or up to four diagnosis codes.
Note: Z codes cannot be your primary diagnosis code if we are billing insurance.
Couples/Family Intakes
In the intake note, the “client” is the individual on the TN chart. The client can be thought of as being treated through the use of either couples or family counseling.
- When writing the intake note, follow the intake note expectations for an individual intake. You can use the name of the client if that is your preference - Jane, or you can use, The Client
For the diagnosis - The diagnosis needs to be about the client (the person in the TN file) only. Diagnoses of the other person do not belong in the intake note.
Couples/Family Diagnosis Examples
Example 1:
F438 - Other Specified Trauma- and Stressor-Related Disorder
Z630 - Relationship Distress with Spouse or Intimate Partner
F43.8 - This diagnosis has been given due to the client's (client's name) symptoms, including anger, frustration, low mood, and difficulty completing tasks related to the stressor of her husband's most recent deployment, as well as their financial stress.
The second diagnosis was given due to the client's disclosure of symptoms, including difficulty communicating effectively, difficulty understanding one another, and disagreements regarding what choices to make for their relationship.
Example 2:
F430 - Adjustment Disorder, Unspecified
Z630 - Relationship Distress with Spouse or Intimate Partner
The clients report symptoms of adjustment disorder, unspecified, in the form of distress related to relationship and communication issues. This distress developed in response to and less than 3 months after their current relationship and communication issues began, and has persisted for fewer than 6 months after onset. This clinician evaluates the client’s expressed distress of symptoms as out of proportion to the severity or intensity of the stressor and causing significant impairment in social and occupational functioning. This clinician evaluates these symptoms as not representing normal bereavement. The client does not meet the criteria for another disorder at this time.
Reassessment at 1 year
During the training from Medicaid, we found out that we are supposed to be conducting a "reassessment" with our clients at the one-year mark for clients who are continuing treatment past that point. (This does not apply to clients who terminate before 1 year). Here are the steps:
- At the 1-year mark, schedule the client for an intake session.
- Treat the session as if it were your first initial session with the client and collect all of the necessary information to complete an intake note (assessment).
- You can use the original intake note and copy and paste any information that has stayed the same from the original intake. For example, the Family History section, Developmental History, and Legal History could be some sections that have not changed.
- Update all sections of the note that contain new information, specifically focusing on the clinical data of current symptoms (presenting problem), current medical necessity (using symptom onset, frequency, duration, severity, and impact on functioning), and current diagnosis (using DSM language and making it person-centered).
- Complete the note and submit it as you normally would.
- The last step would be to update the Treatment Plan to reflect any new changes that affect what you and the client are working on currently.
You do not need to have the client fill out all of the initial paperwork they did as a new client. The only document that needs to be signed again is:
- ROI's that are past the 1-year mark.
This is the actual wording from Medicaid about a Reassessment:
- "Reassessment - Psychiatric diagnostic evaluation is an integrated biopsychosocial assessment, including history, mental status, presenting concerns, determining diagnosis/diagnoses, baseline level of functioning, determining appropriate level of care or treatment needs, and making recommendations and necessary referrals or open to treatment."