Billable Diagnosis
The #1 cause of denial from insurance is billing a non billable diagnosis.
The table below lists the covered diagnoses under the Colorado Capitated Behavioral Health Benefit under the Accountable Care Collaborative. OBH also covers the diagnosis codes listed below. Additionally, in an effort to provide early intervention services to the “non-targeted” children’s population (ages zero to eleven), OBH will allow for BH codes not listed below. “Non-targeted” children are defined as those not meeting the Severe Emotional Disturbance definition as defined through the Colorado Client Assessment Record (CCAR) Manual or COMPASS Rules Manual. OBH is allowing for a broader range of diagnosis codes for “Non-targeted” children in an effort to provide services to children who are at risk of developing a severe diagnosis and/or who are difficult to diagnose as a result of their age.
Billable / Covered Diagnoses Ranges
SUD Diagnosis needs to be billed in the Secondary Position for CCHA (Medicaid)
When billing the most common mental health service codes (90791, 90837, 90832, 90834…) to CCHA, a mental health dx needs to be billed in the primary position and the SUD dx would need to be placed in the second position.
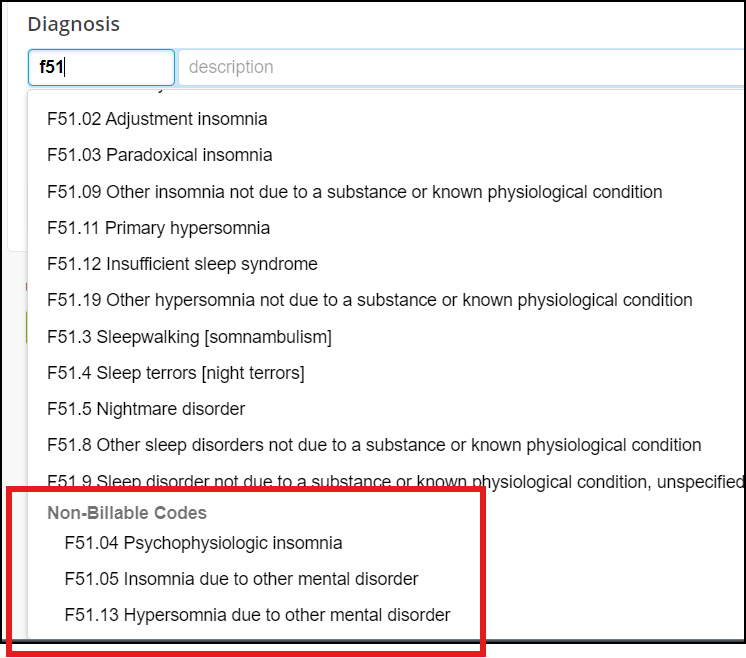
Non-Billable Dx in TN
As you search ICD-10 codes in TN, you see non-billable codes. Some non-billable codes are:
- F43.8 is a non-billable diagnosis. Use F43.81 or .89.
Non-Covered Diagnosis
A covered diagnosis is required for reimbursement, unless it falls in one of the following categories: Screening, Assessment, Crisis, or Prevention/Early Intervention. (See Appendix B and Appendix C for specific codes allowed without a covered diagnosis.) For these services, a non-covered diagnosis may be reported when these services have been rendered to a Medicaid enrollee for the purpose of evaluating and assessing to determine the presence of and/or diagnose a BH disorder(s). When no other diagnosis has been determined, R69 or Z03.89 may be used. These codes are specifically intended for use when persons without a diagnosis are suspected of having an abnormal condition, without signs or symptoms, which requires study, but after examination and observation, is found not to exist.
